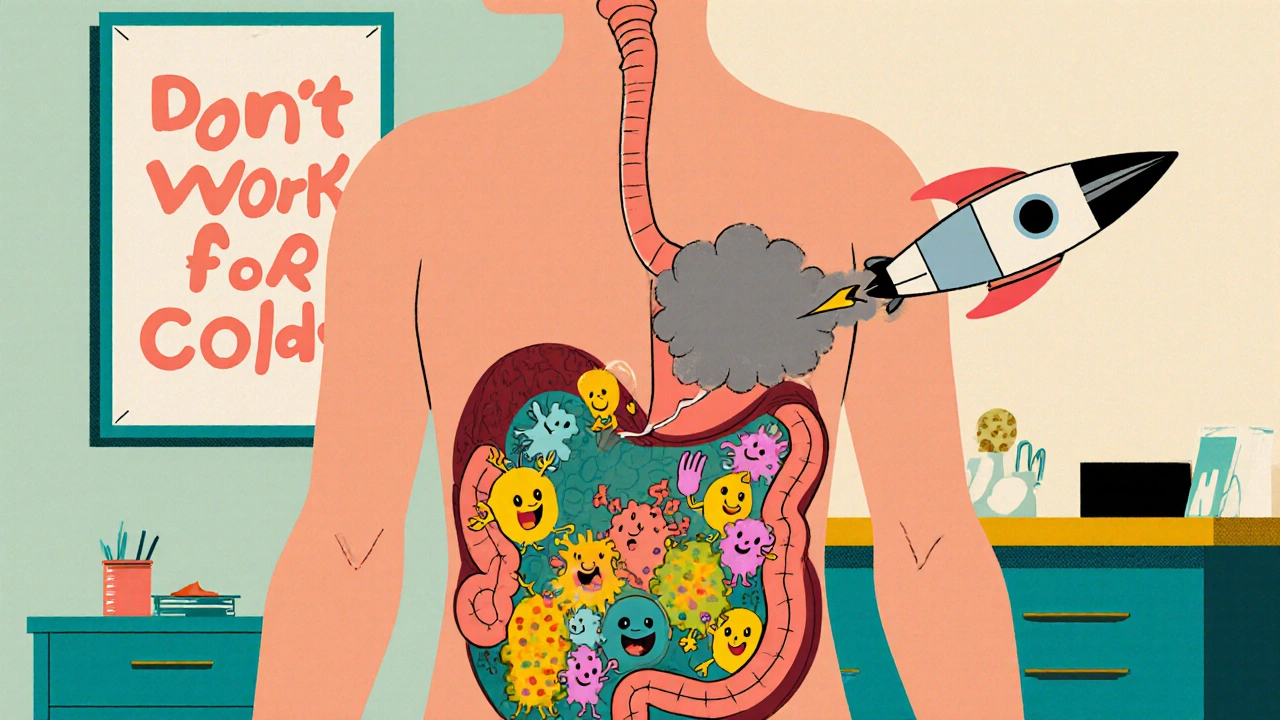
Every time you take an antibiotic, you’re not just fighting an infection-you’re changing the entire ecosystem inside your gut. Most people don’t realize that antibiotics don’t just kill the bad bacteria causing your sore throat or sinus infection. They also wipe out the good ones-the trillions of helpful microbes that keep your digestion running, your immune system sharp, and your body protected from dangerous invaders like Clostridioides difficile (C. diff). This is why antibiotic stewardship isn’t just a hospital policy or a doctor’s checklist. It’s personal. It’s about making sure you only get antibiotics when they’re truly needed, and when you do, that you get the right one, at the right dose, for the right amount of time.
Why Antibiotic Stewardship Matters More Than Ever
More than 2.8 million antibiotic-resistant infections happen in the U.S. every year. Over 35,000 people die from them. That’s not a distant statistic-it’s someone you know. The CDC calls antimicrobial resistance one of the top 18 public health threats we face. And the biggest driver? Overuse. Not just in hospitals, but in doctor’s offices, urgent care centers, and even through over-the-counter sales in some countries.
Here’s the hard truth: about 46% of antibiotic prescriptions for acute respiratory infections-like colds, bronchitis, and sinus infections-are unnecessary. Viruses cause most of these. Antibiotics do nothing to them. Yet, patients often expect them. Doctors sometimes give them to avoid conflict or because they’re rushed. That’s where stewardship steps in-not to restrict, but to guide.
How Antibiotic Stewardship Protects Your Gut
Your gut is home to more bacteria than there are stars in the Milky Way. These microbes help break down food, make vitamins, train your immune system, and block harmful bugs from taking over. Antibiotics don’t distinguish between friend and foe. A single course can wipe out 30-40% of your gut’s good bacteria-and it can take months, sometimes years, for them to bounce back. In some cases, they never fully recover.
This disruption creates a vacuum. One of the first invaders to move in? C. diff. It’s not rare. About 1 in 5 people who take antibiotics develop C. diff infection. That means diarrhea, fever, abdominal pain-and in severe cases, colon damage, sepsis, or death. In the U.S., C. diff causes more than 223,000 infections and 12,800 deaths each year. And antibiotics are the #1 risk factor.
Antibiotic stewardship cuts this risk by reducing unnecessary use. At hospitals like the University of Nebraska Medical Center, where stewardship has been active since 2004, C. diff rates dropped by nearly 40% after implementing strict prescribing guidelines. The key? Not avoiding antibiotics altogether-but using them smarter.
The Core Elements of a Successful Stewardship Program
Effective stewardship isn’t magic. It’s a system. The CDC’s Core Elements framework breaks it down into seven parts:
- Leadership commitment: Hospitals and clinics must dedicate time, staff, and money to stewardship.
- Accountability: Someone-usually an infectious disease doctor or pharmacist-must be in charge.
- Drug expertise: Pharmacists trained in infectious diseases review every antibiotic order.
- Action: Programs use tools like pre-authorization, prospective audit, or the more personal “handshake stewardship.”
- Tracking: They measure how many antibiotics are used (days of therapy per 1,000 patient days) and what happens after (C. diff rates, readmissions).
- Reporting: Doctors get feedback: “You prescribed 30% more amoxicillin than your peers last month.”
- Education: Staff and patients learn when antibiotics help and when they don’t.
One of the most effective methods? “Handshake stewardship.” Instead of blocking prescriptions, a pharmacist and doctor walk into a nurse’s station and say, “Hey, I noticed you prescribed ciprofloxacin for this urinary tract infection. Have you considered nitrofurantoin? It’s just as effective, cheaper, and much gentler on the gut.” No red tape. No refusal. Just conversation. Studies show this approach increases consults, reduces resistance, and saves hospitals over $2 million a year.

What Happens in Outpatient Settings?
Most antibiotics are prescribed outside hospitals-in clinics, urgent cares, pediatric offices. That’s where the biggest opportunities lie.
Doctors treating kids with ear infections? Many still prescribe 10-day courses of amoxicillin, even though studies show 5-7 days work just as well. For strep throat? Antibiotics are necessary. For coughs, colds, or runny noses? Almost never.
Outpatient stewardship uses simple, powerful tools:
- Computer alerts that pop up when a doctor tries to prescribe antibiotics for viral symptoms.
- Posters in exam rooms with messages like: “Antibiotics don’t work for colds. Let’s talk about what will help.”
- Peer comparison reports: “You prescribe antibiotics for bronchitis 2.5 times more than your colleagues.”
One study found that just putting a commitment poster in an exam room reduced inappropriate prescribing by 5.6%. That’s not a lot-but multiply that across thousands of clinics, and you’re talking about hundreds of thousands of fewer antibiotic courses each year.
Who’s Leading the Charge?
It’s not just doctors. It’s pharmacists, nurses, hospital administrators, and even patients. The Joint Commission made antibiotic stewardship a mandatory safety goal in 2020. That means every accredited U.S. hospital must have a program. As of 2022, 84% of large hospitals had one. But only 54% of smaller hospitals did. That’s where gaps remain.
Specialists like infectious disease physicians and clinical pharmacists are the backbone. They’re trained to know which antibiotic kills which bug, how long to treat it, and which ones spare the gut microbiome. The American Academy of Pediatrics updated its guidelines in 2020 to reflect that kids aren’t just small adults-their infections, their drug metabolism, and their gut resilience are different. That’s why pediatric stewardship programs now recommend shorter courses for ear infections, tonsillitis, and pneumonia.

What’s Next? AI, Diagnostics, and Precision
The future of stewardship is faster, smarter, and more personal. New rapid tests can now tell if an infection is bacterial or viral in under an hour-instead of waiting 2-3 days for cultures. Some hospitals are using AI tools that analyze patient charts in real time and suggest the best antibiotic based on local resistance patterns, kidney function, allergies, and even recent antibiotic use.
One pilot program at a major academic medical center cut inappropriate prescribing by 18% using AI alerts. These tools don’t replace doctors-they help them make better decisions faster.
And it’s not just about choosing the right drug. It’s about choosing the right duration. New research shows that for many infections-like urinary tract infections, pneumonia, and skin infections-shorter courses (5-7 days) are just as effective as 10-14 days. Less drug. Fewer side effects. Less damage to the gut.
What You Can Do
You don’t need to be a doctor to be part of the solution. Here’s how you can protect yourself and your family:
- Ask: “Do I really need this antibiotic?” If your doctor says “it’s just a virus,” believe them.
- Don’t pressure for antibiotics. Cold? Flu? Cough? Antibiotics won’t help. Rest, fluids, and time will.
- Take exactly what’s prescribed. No skipping doses. No saving leftovers. No giving them to someone else.
- Ask about duration. “Is a 5-day course enough?” Many infections don’t need 10 days.
- Consider probiotics after antibiotics. Not all are equal. Look for strains like Lactobacillus rhamnosus or Saccharomyces boulardii, shown in studies to reduce C. diff risk.
Antibiotics are lifesavers. But they’re not harmless. Every time we use them carelessly, we risk losing them forever. And when they stop working, common infections become deadly again. Stewardship isn’t about saying no to antibiotics. It’s about saying yes-wisely.
What Happens If We Don’t Act?
If we keep overusing antibiotics, we’re heading toward a world where even minor surgeries, chemotherapy, or a scraped knee can turn deadly. A simple urinary tract infection could require a hospital stay. A child’s ear infection might need surgery. We’ve already seen this happen in parts of the world where resistance is rampant.
The CDC estimates that if we scale up stewardship nationwide, we could prevent 130,000 C. diff infections and save 10,000 lives by 2025. That’s not a guess. That’s a projection based on data from hospitals that have already done it.
Protecting your gut isn’t just about eating yogurt. It’s about asking the right questions before you fill a prescription. Because the next time you need an antibiotic, you’ll want one that still works-and a gut that still works with it.

David vaughan
November 22, 2025 AT 11:30Wow. This is one of those posts that makes you pause and actually think. I had no idea antibiotics could wreck your gut microbiome for years. I used to always ask for them when I had a cold... now I’m gonna hold off and see if it clears up on its own. Thanks for the wake-up call.
Daisy L
November 24, 2025 AT 09:51AMERICA NEEDS TO STOP BEING LAZY ABOUT HEALTH. We don’t need antibiotics for every sniffle. We need discipline. We need backbone. And we need to stop treating doctors like vending machines for pills. This is why we’re losing the war on superbugs - because people want quick fixes, not real solutions.
Corra Hathaway
November 25, 2025 AT 18:38YESSSSS. I’ve been saying this for years 😌💪 My kid had an ear infection last year and the doc said ‘let’s wait 48 hours’ - guess what? It cleared up on its own. No antibiotics. No drama. Just patience. And yes, I’m still taking probiotics. 🤓
Noah Fitzsimmons
November 26, 2025 AT 23:31Oh wow, so now we’re supposed to trust doctors who barely spend 5 minutes with us? LOL. You really think they care about your gut flora? Nah. They’re paid by Big Pharma to push pills. The ‘handshake stewardship’? Cute. It’s all PR. The real agenda? Keep you dependent on meds. 🤡
Michael Marrale
November 28, 2025 AT 09:38Did you know the government’s been secretly spraying antibiotics into the water supply since 2012? They say it’s for ‘public health’ but it’s really to control our microbiomes so we don’t rebel. I’ve been drinking filtered rainwater since then. My gut’s never been better. Also, the CDC is a CIA front. Ask yourself: why are they so obsessed with C. diff? 😈
David Cusack
November 28, 2025 AT 10:02How quaint. A 12-page manifesto on stewardship, yet not a single citation to the 2023 Lancet meta-analysis on microbiome recovery timelines. One assumes the author has never read a peer-reviewed paper, let alone encountered the concept of ‘effect size.’ The anecdotal ‘handshake’ approach is charming, but statistically insignificant. One wonders if the author conflates sentiment with science.
Eliza Oakes
November 29, 2025 AT 04:34Okay but what if I just WANT the antibiotic? Like… what if I’m tired of feeling sick and I don’t care about the ‘ecosystem’? My body, my choice. You’re not my microbiome police. Also, I read somewhere that probiotics are a scam. So now I’m supposed to suffer and take vitamins? No thanks.
Clifford Temple
December 1, 2025 AT 01:24Why are we letting foreigners dictate our healthcare? We’ve got the smartest doctors in the world. Why are we copying some EU policy? We don’t need ‘handshakes’ - we need strong leadership. And stop telling Americans what to do. We know our bodies better than some pharmacist in Nebraska.
Paula Jane Butterfield
December 2, 2025 AT 00:40Just wanted to say THANK YOU for this post!! 🙏 I’m a nurse and I see this every day - parents begging for antibiotics for a runny nose. I show them the CDC posters and they still look confused. You’re right - it’s about education, not force. I’m printing this out and putting it in my clinic. You’re doing the work 💛
Shawn Sakura
December 2, 2025 AT 12:25So… if you take an antibiotic, and then take a probiotic… does that count as ‘smart prescribing’? I mean, I’ve been doing that for years. Also, I think I spelled ‘probiotic’ wrong. Sorry. But I’m trying. 😅
Simone Wood
December 4, 2025 AT 11:10Antibiotic stewardship? More like antibiotic suppression. The pharmaceutical-industrial complex has been weaponizing microbiome science for profit since the 90s. You think C. diff is a ‘side effect’? It’s a feature. The real threat isn’t resistance - it’s loss of control. And the ‘handshake’? That’s just corporate speak for ‘we’re still selling you pills, just slower.’
Swati Jain
December 4, 2025 AT 15:09As someone from India, where antibiotics are sold over the counter like candy - this is GOLD. We need this in every village clinic. My cousin died from C. diff after a 10-day course of cipro for a ‘stomach bug.’ No culture. No test. Just ‘take this.’ We need training. We need systems. Not just posters. Real change.
Anne Nylander
December 6, 2025 AT 00:25YOU GOT THIS. 💪 Every time you say ‘no’ to an unnecessary antibiotic, you’re saving lives - including your own. It’s not easy, but you’re stronger than you think. And yes, your gut will thank you. Start small. Ask one question. That’s all it takes. You’re already making a difference. ❤️