When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. That’s the whole point of bioequivalence - it’s the scientific guarantee that the generic delivers the same medicine, at the same rate, to your body. But what if the batch of generic pills you’re holding isn’t even the same as the one tested in the lab? What if the brand-name drug itself varies from batch to batch, and no one’s checking for that? This isn’t theory. It’s a real, documented problem in generic drug approval - and it’s changing how regulators and manufacturers think about safety.
What Bioequivalence Actually Means
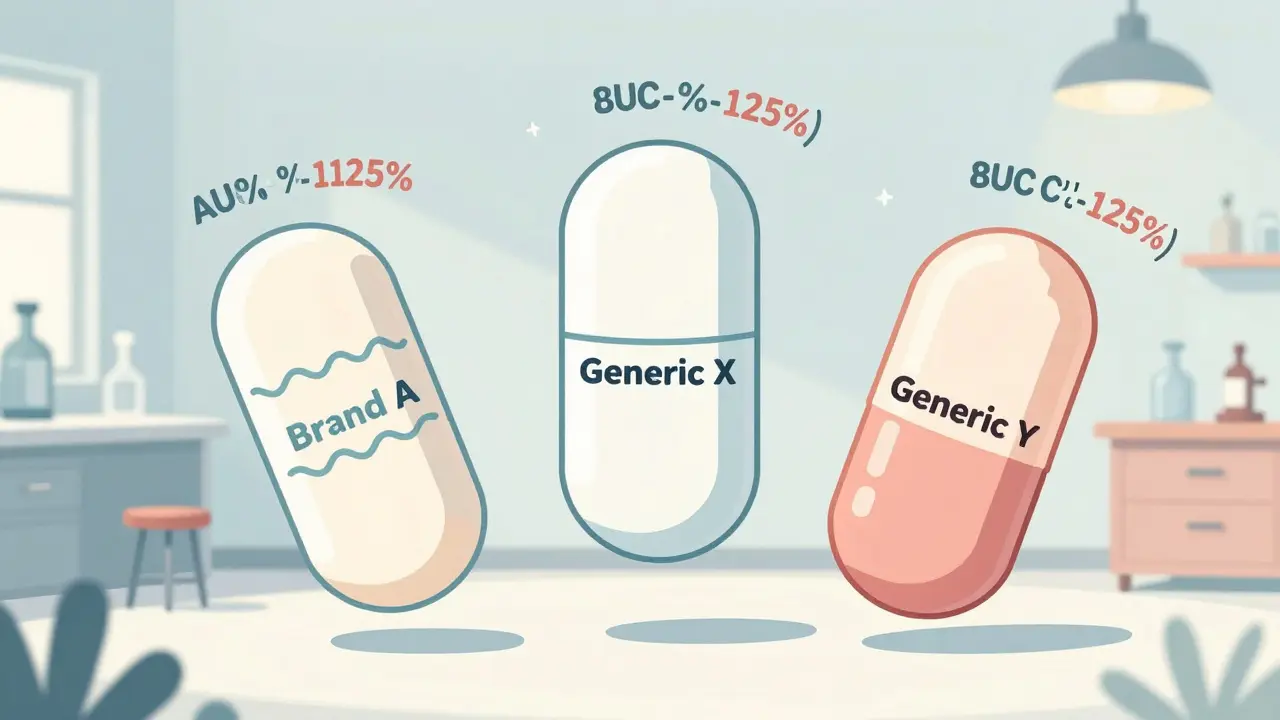
Bioequivalence isn’t about matching ingredients. It’s about matching how your body absorbs the drug. Two drugs are considered bioequivalent if their key measurements - AUC (total exposure) and Cmax (peak concentration) - fall within 80% to 125% of each other. This range was set by the FDA in 1992 and later adopted worldwide. It sounds simple. But here’s the catch: this test is usually done using just one batch of the generic and one batch of the brand-name drug.
That’s like testing two cars for fuel efficiency using one tank of gas from each, then saying all tanks from both brands are identical. But in reality, manufacturing isn’t perfect. Even the same company making the same drug can have slight differences between batches - changes in particle size, coating thickness, or mixing uniformity. These small shifts can change how fast the drug dissolves in your stomach. And when those differences aren’t accounted for, the bioequivalence result might be misleading.
Why Batch Variability Is a Hidden Problem
A 2016 study in Clinical Pharmacology & Therapeutics found that between-batch variability accounts for 40% to 70% of the total error in bioequivalence studies. That means most of the "noise" in the data isn’t from people’s bodies reacting differently - it’s from the drugs themselves being slightly different.
Take a nasal spray. A tiny change in how the liquid is pressurized or how the particles are sized can drastically affect how much medicine reaches your lungs. But under current rules, if one batch of the generic passes bioequivalence testing against one batch of the brand, it’s approved - even if other batches of the generic or brand vary more than expected.
Imagine two generic brands both pass the 80-125% test. But one was tested against a low-variability batch of the brand, while the other was tested against a high-variability batch. The first might be safe. The second could be inconsistent - but you’d never know. That’s what experts call "confounded bioequivalence" - where the result tells you more about the batches used than the products themselves.
The Current System Is Built on a Flaw
The standard method, called Average Bioequivalence (ABE), ignores batch variability entirely. It assumes all batches are identical. But data shows they’re not. A 2019 presentation by Dr. Robert Lionberger, former head of the FDA’s Office of Generic Drugs, called this "one of the most significant statistical oversights" in modern drug approval.
Here’s how it breaks down:
- ABE compares one test batch to one reference batch.
- If the results fall within 80-125%, the generic is approved.
- But if the reference batch used in testing was unusually consistent, the confidence interval looks tighter than it should - making the generic look better than it really is.
- If the reference batch was highly variable, the interval gets wider, and a perfectly good generic might fail - even though it’s actually equivalent.
This isn’t just theoretical. The FDA reported a 22% increase in bioequivalence-related deficiencies in generic drug applications between 2019 and 2022. Many of those were because companies didn’t test enough batches or didn’t show how consistent their manufacturing was.
What’s Changing: The Rise of Between-Batch Bioequivalence (BBE)
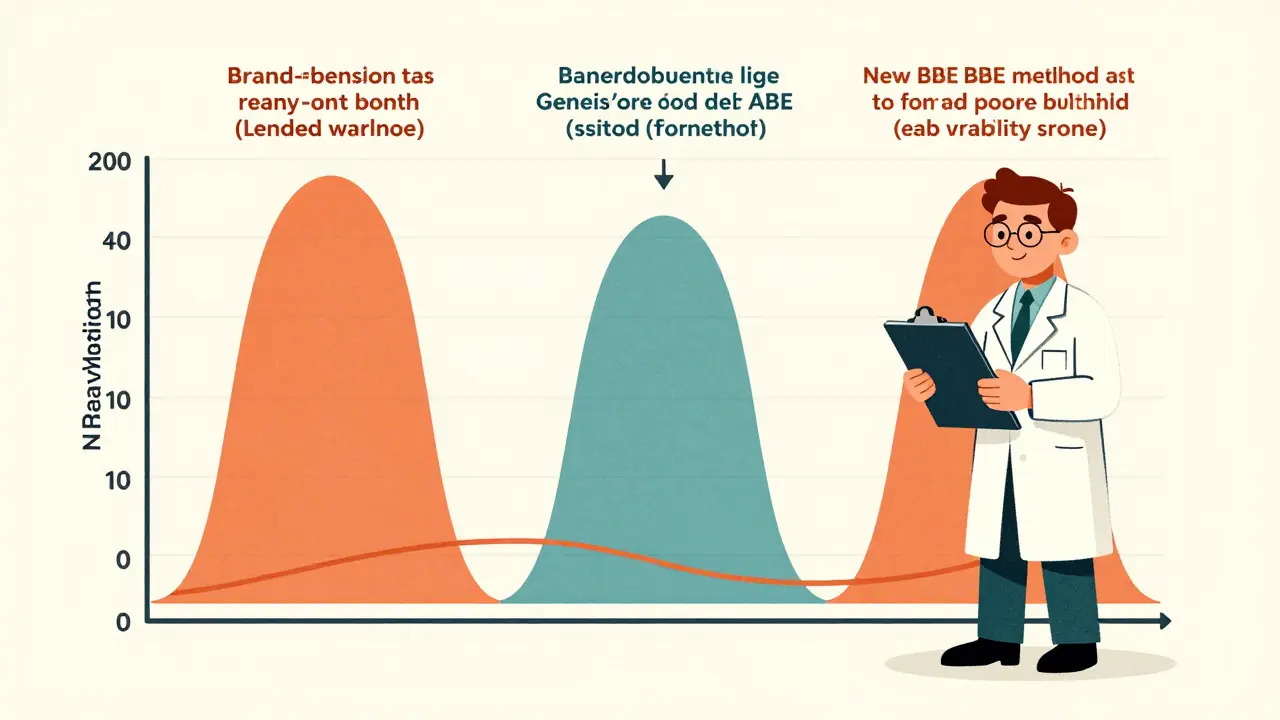
A new approach is gaining ground: Between-Batch Bioequivalence (BBE). Instead of comparing the generic to one brand batch, BBE compares it to the range of variability seen in the brand’s own batches.
Here’s how it works:
- Test at least three batches of the brand-name drug.
- Calculate the standard deviation of their AUC and Cmax values.
- Test two or more batches of the generic.
- Compare the average difference between the generic and the brand to twice the brand’s between-batch standard deviation.
- If the difference is smaller than that threshold, the generic is approved.
This method doesn’t require more people in the study - just more batches of the drug. And it’s smarter. It says: "We’re not just matching one sample. We’re matching the entire performance range of the original product."
Simulations show that with just three reference batches, BBE correctly identifies true bioequivalence 65% of the time. With six batches, that jumps to over 85%. That’s a massive improvement over the current system.
Regulators Are Catching Up
Regulatory agencies are starting to respond. The FDA released a draft guidance in June 2023 titled Consideration of Batch-to-Batch Variability in Bioequivalence Studies. It’s not law yet, but it signals a shift. The EMA held a workshop in 2023 and listed "inadequate consideration of batch variability" as one of the top three challenges in generic drug development.
Some products are already being held to higher standards. For example, the FDA now requires applicants for nasal sprays to provide data from at least three production-scale batches of both test and reference products. That’s a direct response to the fact that inhalers and sprays are especially sensitive to manufacturing changes.
The European Federation for Pharmaceutical Sciences (EUFEPS) called for immediate action in 2021. And the International Council for Harmonisation (ICH) is developing new guidelines (Q13) that will push manufacturers to prove consistency across production scales - especially with new continuous manufacturing technologies.
What This Means for You
For patients: you’re still getting safe, effective generics. The system works most of the time. But the fact that batch variability is now being openly discussed means regulators are finally addressing a hidden risk. In the future, you might see more detailed labeling or public reports on batch consistency - especially for critical drugs like blood thinners, seizure medications, or asthma inhalers.
For prescribers: know that not all generics are created equal in terms of manufacturing rigor. If a patient has a strange reaction after switching generics, it’s not always about individual sensitivity. It could be a batch difference.
For manufacturers: the bar is rising. Companies that only test one batch will struggle to get approval. Those investing in multi-batch testing and statistical modeling will lead the market.
The Future: Multi-Batch Testing Will Be the Norm
By 2025, experts predict that bioequivalence studies for complex generics - like inhalers, injectables, or topical creams - will require at least three reference batches and two test batches. The old "one batch, one test" rule will be phased out for high-risk products.
Dr. Jennifer Bright of the Critical Path Institute says the next five years will see a "fundamental shift" from single-batch to multi-batch frameworks. And she’s right. The data is clear: ignoring batch variability isn’t just outdated - it’s risky.
The 80-125% rule was a breakthrough in the 1990s. But today’s manufacturing, with its precision and complexity, demands a smarter standard. The goal isn’t just to prove equivalence - it’s to prove consistent, reliable equivalence, batch after batch. That’s what patients deserve. That’s what science now requires.
What does "bioequivalence" mean for generic drugs?
Bioequivalence means that a generic drug delivers the same amount of active ingredient into the bloodstream at the same rate as the brand-name version. This is measured using two key values: AUC (total exposure) and Cmax (peak concentration). If the ratio of these values between the generic and brand falls between 80% and 125%, the drugs are considered bioequivalent and legally interchangeable.
Why does batch variability matter in bioequivalence testing?
Batch variability means that even the same drug made by the same company can differ slightly between production runs. These differences - in particle size, coating, or mixing - can affect how quickly the drug is absorbed. If bioequivalence is tested using only one batch of each product, the result may not reflect the true performance of the entire product line. Studies show batch variability can make up 40-70% of the error in these tests, leading to false approvals or unnecessary rejections.
Is the 80-125% bioequivalence range still valid?
Yes, but it’s incomplete. The 80-125% range is still the official standard for most drugs. However, it doesn’t account for differences between manufacturing batches. Experts agree that while the range works for simple, stable drugs, it’s inadequate for complex products like inhalers, nasal sprays, or injectables. New methods like Between-Batch Bioequivalence (BBE) are being developed to fix this gap.
What is Between-Batch Bioequivalence (BBE)?
BBE is a new statistical method that compares a generic drug’s average performance to the natural variability of the brand-name drug across multiple batches. Instead of matching one batch to another, BBE asks: "Is the generic as consistent as the original?" It uses the brand’s own batch-to-batch standard deviation as a benchmark. If the difference between generic and brand is less than twice that standard deviation, the generic is approved. This approach is more accurate for variable products.
Which drugs are most affected by batch variability?
Drugs with complex delivery systems are most affected. These include inhalers, nasal sprays, topical creams, injectables, and extended-release tablets. Small changes in manufacturing - like spray nozzle size or coating thickness - can significantly alter how the drug is absorbed. For these products, batch variability can make the difference between effective treatment and treatment failure.
Are generic drugs still safe to use?
Yes. The vast majority of generic drugs are safe and effective. Regulatory agencies approve thousands of generics each year with strong safety records. But the growing focus on batch variability means future approvals will be more rigorous - especially for high-risk products. This isn’t a warning to avoid generics. It’s a step toward making them even more reliable.

Jane Lucas
December 27, 2025 AT 09:50Just had to switch my generic blood pressure med last month and my head felt like a balloon for a week. Not sure if it was the batch or my nerves but now I check the label like a hawk.
Kylie Robson
December 27, 2025 AT 22:06Let’s be clear - the ABE paradigm is statistically underpowered for heterogeneous formulations. The 80-125% CI is a population-level heuristic that fails to capture intra-individual PK variance when compounded by inter-batch manufacturing sigma > 10%. BBE introduces a variance-component model that aligns with ICH Q13’s process analytical technology (PAT) framework - finally, a move toward process capability, not just product equivalence.
Caitlin Foster
December 29, 2025 AT 20:04So let me get this straight - we’ve been letting Big Pharma and the FDA skate on ONE BATCH of testing for 30 years?? 😳 Like, I could make a cookie recipe with 3 different flours and call them all ‘chocolate chip’ but you’d still know the texture was off. Why are we treating life-saving meds like a baking experiment??
Elizabeth Alvarez
December 31, 2025 AT 11:00They don’t want you to know this but the real reason they ignore batch variability is because the FDA is secretly owned by the brand-name pharma conglomerates. They profit off you switching generics and getting sick because the new batch doesn’t match. Then they sell you the brand again at triple the price. It’s not incompetence - it’s intentional. They’ve been doing this since the 90s. The ‘draft guidance’? A distraction. The real test is whether they’ll force companies to publish batch-level data publicly - they won’t. Because then you’d see how many generics are just sugar pills with a fancy label.
Miriam Piro
January 2, 2026 AT 00:37Think about it - we trust our lives to a pill that’s approved based on a single sample like it’s a lottery ticket. 🤡 The system isn’t broken - it’s designed to make you feel safe while quietly gambling with your biochemistry. They call it ‘bioequivalence’ but what they really mean is ‘close enough for government work.’ And now they’re gonna fix it with… more paperwork? LOL. The real solution? Ban generics entirely. Or make every batch traceable to a blockchain. Or at least let us see the batch number and look up its test results. But nah. Too much transparency. Too much accountability. We’re just patients. We’re not supposed to ask questions. 😌
dean du plessis
January 3, 2026 AT 19:44Interesting read. I work in a clinic in Cape Town and we rely on generics for 90% of our prescriptions. Most patients do fine but I’ve seen a few cases where switching brands caused issues - especially with epilepsy meds. Never thought it could be batch variation until now. Makes sense to test more than one batch. Simple fix really.
Todd Scott
January 4, 2026 AT 22:06As someone who’s worked in pharma QA for 18 years, I’ve seen this play out firsthand. Back in 2010, we had a generic anticoagulant that passed ABE with flying colors - but when we ran a multi-batch stability study, one batch had a 15% lower Cmax due to a coating change no one flagged. Patient had a minor bleed. We had to recall. The FDA didn’t require that test. We did it because we were paranoid. Now? They’re finally catching up. BBE isn’t magic - it’s just good science. And honestly? It’s cheaper long-term. Fewer recalls, fewer lawsuits, fewer scared patients. The real resistance? From companies that don’t want to invest in consistent manufacturing. Not the regulators.
Andrew Gurung
January 6, 2026 AT 05:00Oh wow. So the entire foundation of generic drug approval is built on a 30-year-old statistical illusion? 🤦♂️ And we’re still letting people take these pills? I mean, if this was a car, you’d be sued for manslaughter. This isn’t just a flaw - it’s a national health scandal. The FDA is basically saying, ‘Trust us, we did a test once.’ And we’re all just nodding like sheep. Meanwhile, people are dying because a batch of levothyroxine had a 5% variance in dissolution rate. And you know what? They still won’t tell you which batch you got. Because transparency = liability. And liability = bad for stock prices. 😔