When you’re hunting for a reliable anti‑nausea drug, Compazine (Prochlorperazine) is a phenothiazine antipsychotic that doubles as a potent anti‑emetic, commonly prescribed for severe nausea, vomiting, and certain psychiatric conditions. It’s been on the market for decades, but newer agents and older generics often pop up as cheaper or better‑tolerated options. This guide breaks down how Compazine stacks up against the most frequently mentioned alternatives, what makes each drug tick, and which factors matter most when you or a loved one need to pick a medication. By the end you’ll know exactly when Compazine shines, when another drug might be smarter, and how to avoid the side‑effects that trip up many patients.
How Compazine Works - The Pharmacology in Plain English
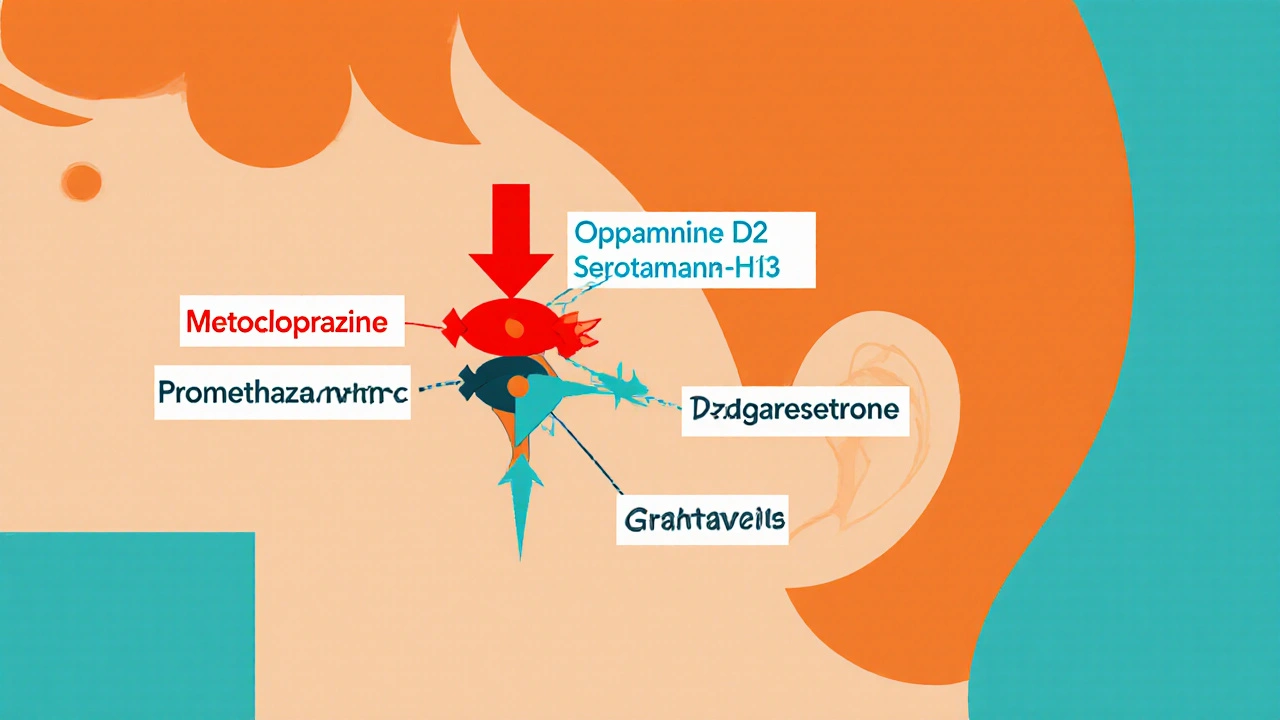
Compazine belongs to the Dopamine antagonist class, meaning it blocks dopamine receptors in the brain’s chemoreceptor trigger zone (CTZ). When dopamine can’t activate those receptors, the nausea signal gets muted. The drug also has modest antihistamine and anticholinergic activity, which adds a mild sedative feel that some patients appreciate during a bout of motion sickness.
Because it targets dopamine, Compazine can help with symptoms that stem from the basal ganglia, such as the tremor‑like movements seen in Parkinson’s disease. That overlap explains why neurologists sometimes prescribe it off‑label for migraine‑associated nausea, even though it isn’t the first‑line choice for that condition.
Top Alternatives to Compazine
Below are the four anti‑nausea medicines that most clinicians compare with Compazine when they write a prescription. Each one hits a different molecular target, which leads to a distinct side‑effect profile and set of approved uses.
Metoclopramide - The Pro‑Motility Option
Metoclopramide is a dopamine D2 receptor antagonist that also stimulates gastrointestinal motility. It’s often the go‑to for chemotherapy‑induced nausea because it works both in the brain and the gut. Unlike Compazine, Metoclopramide can cause a rare but serious movement disorder called tardive dyskinesia when used long‑term.
Promethazine - The Histamine Blocker
Promethazine is a first‑generation antihistamine with strong anti‑emetic and sedative properties. It’s popular for motion sickness and postoperative nausea. Its heavy antihistamine action can make you drowsy, which some patients actually want after surgery, but it’s a deal‑breaker for anyone who needs to stay alert.
Ondansetron - The Serotonin 5‑HT3 Blocker
Ondansetron is a selective serotonin 5‑HT3 receptor antagonist used primarily for chemotherapy, radiation, and surgery‑related nausea. Because it doesn’t touch dopamine, it avoids many of the extrapyramidal side effects that trouble Compazine users. However, it can cause constipation and, in rare cases, cardiac rhythm changes.
Granisetron - Another 5‑HT3 Antagonist
Granisetron is a long‑acting serotonin 5‑HT3 antagonist often given as a transdermal patch for chronic nausea. It shares Ondansetron’s mechanism but offers a smoother dosing schedule, which is handy for patients on ongoing chemotherapy.
Side‑Effect Snapshot - What to Expect
Side‑effects are the real deal‑breakers when you compare drugs. Below is a quick cheat‑sheet that highlights the most common and concerning adverse events for each medication.
- Compazine (Prochlorperazine): Drowsiness, dry mouth, blurred vision, extrapyramidal symptoms (like muscle stiffness or tremor), and rare neuroleptic malignant syndrome.
- Metoclopramide: Restlessness, insomnia, tardive dyskinesia (with long use), and mild diarrhea.
- Promethazine: Strong sedation, anticholinergic effects (dry mouth, urinary retention), and rare severe skin reactions.
- Ondansetron: Constipation, headache, and occasional QT‑prolongation on an ECG.
- Granisetron: Constipation, injection site pain (if given IV), and mild dizziness.
Direct Comparison Table
| Medication | Mechanism | Typical Uses | Common Side Effects | Key Difference vs. Compazine |
|---|---|---|---|---|
| Compazine (Prochlorperazine) | Dopamine D2 antagonist | Severe nausea, vomiting, migraine‑associated nausea, psychosis | Drowsiness, dry mouth, extrapyramidal symptoms | Strong antipsychotic action, higher risk of movement disorders |
| Metoclopramide | Dopamine D2 antagonist + GI motility enhancer | Chemotherapy nausea, gastroparesis | Restlessness, tardive dyskinesia (long‑term) | Promotes gut movement; less sedating than Compazine |
| Promethazine | Histamine H1 antagonist (plus anticholinergic) | Motion sickness, postoperative nausea | Heavy sedation, dry mouth | More sedating; no dopamine blockade |
| Ondansetron | Serotonin 5‑HT3 antagonist | Chemotherapy, radiation, surgery nausea | Constipation, headache, QT prolongation | No dopamine effects; safer for patients with movement‑disorder risk |
| Granisetron | Serotonin 5‑HT3 antagonist (long‑acting) | Chronic chemotherapy nausea, transplant conditioning | Constipation, mild dizziness | Transdermal option; similar safety to Ondansetron |
Factors to Weigh When Choosing the Right Anti‑Nausea Drug
Picking a medication isn’t just about “which one works best.” You have to line up a few practical considerations.
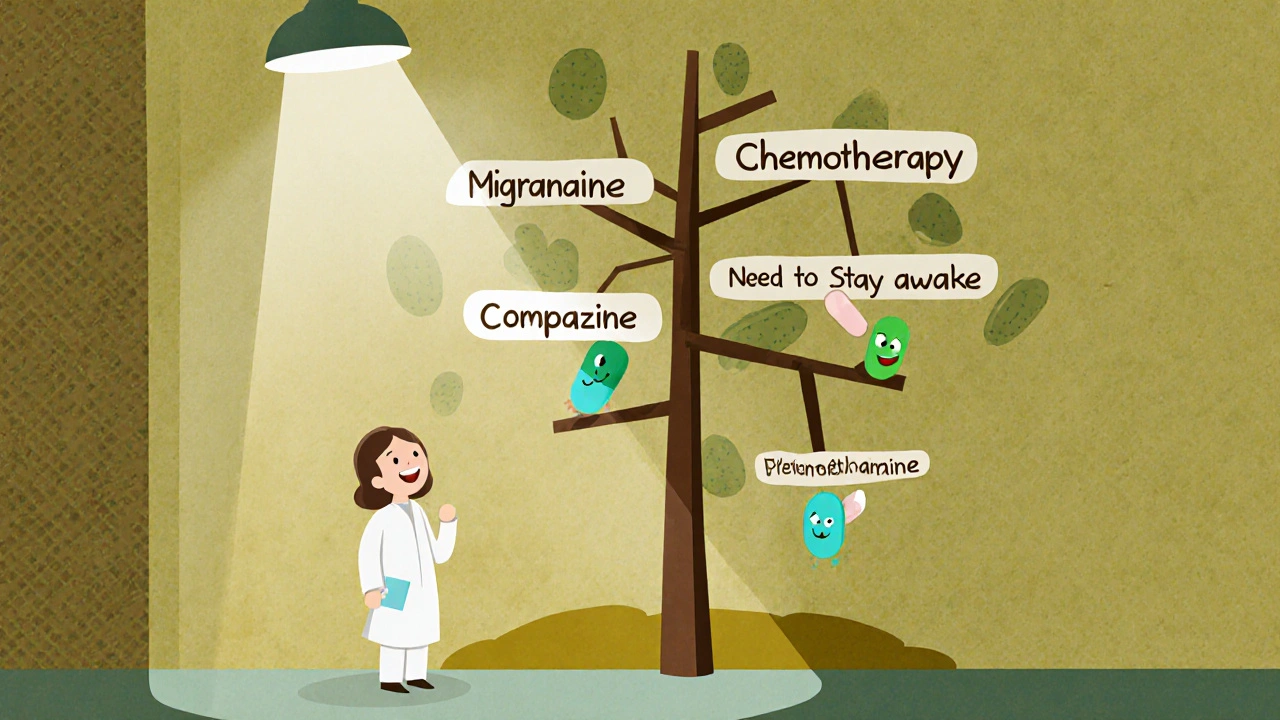
- Underlying cause of nausea: If the nausea is chemo‑related, a 5‑HT3 blocker like Ondansetron usually wins. For migraine‑triggered nausea, Compazine or Metoclopramide are often preferred because they also have some dopamine‑related migraine relief.
- Risk of movement disorders: Patients with Parkinson’s disease or a history of tardive dyskinesia should steer clear of dopamine antagonists (Compazine, Metoclopramide) and lean toward Promethazine or a 5‑HT3 blocker.
- Need for sedation: If you want to stay awake (e.g., during a long drive), avoid Promethazine. If you’re in a post‑op recovery room and want to sleep, its sedative effect is a bonus.
- Drug‑interaction profile: Compazine can heighten the effects of other antipsychotics, while Ondansetron may interact with certain heart medications that affect QT interval. Always run a quick med‑check.
- Cost and insurance coverage: Generic Metoclopramide and Promethazine are often cheaper than branded Compazine, but some plans cover ondansetron without a prior authorization, making it the most affordable 5‑HT3 option for many.
Safety Tips and Red Flags
Regardless of which drug you end up with, keep these safety habits front‑and‑center.
- Never combine two dopamine blockers unless a specialist orders it; the risk of severe extrapyramidal symptoms jumps dramatically.
- If you notice sudden muscle stiffness, facial twitching, or uncontrolled movements, stop the medication and call your doctor immediately - those could be early signs of neuroleptic malignant syndrome (Compazine) or tardive dyskinesia (Metoclopramide).
- Check your heart rhythm if you’re on Ondansetron or Granisetron and you also take other QT‑prolonging drugs like certain antibiotics or anti‑arrhythmics.
- Stay hydrated. Many anti‑nausea meds dry out the mouth and can cause constipation, especially the 5‑HT3 blockers.
- Pregnancy? Discuss with your OB‑GYN. Compazine is Category C, while Ondansetron is Category B in the US, meaning the latter generally has a cleaner safety record for pregnant patients.
When Compazine Still Beats the Rest
Even after the side‑effect rundown, there are scenarios where Compazine is the clear winner.
First, for severe migraine‑related nausea, its dopamine blockade can doubly target the headache pathway, giving faster relief than a pure serotonin blocker. Second, when a patient also needs antipsychotic coverage, Compazine can serve both roles, cutting down on pill burden. Finally, in emergency settings where IV administration is required for rapid control of vomiting, Compazine’s IV formulation works quickly and is widely stocked in hospitals.
Bottom Line: A Practical Decision Tree
To make the choice simpler, follow this quick flowchart:
- Is the nausea caused by chemotherapy or surgery?
Yes → Go with Ondansetron or Granisetron. - Is the patient prone to movement disorders or already has Parkinson’s disease?
Yes → Avoid dopamine antagonists; choose Ondansetron or Promethazine (if sedation is okay). - Is rapid relief needed for migraine‑associated nausea?
Yes → Compazine or Metoclopramide, with a tilt toward Compazine for stronger anti‑migraine effect. - Is cost a primary concern and the patient can tolerate mild sedation?
Yes → Promethazine (generic) or Metoclopramide. - Otherwise, weigh side‑effect tolerance: if you need to stay awake, skip Promethazine; if you want to avoid constipation, skip Ondansetron and Granisetron.
Frequently Asked Questions
Can I use Compazine for motion sickness?
Yes, Compazine works for motion‑induced nausea, but many doctors prefer Promethazine because its stronger antihistamine action often provides better relief with fewer movement‑related side effects.
How quickly does Compazine start working?
When taken orally, you’ll feel a reduction in nausea within 30‑60 minutes. IV dosing can work within 5‑10 minutes, making it a good choice in emergency rooms.
What is the biggest safety concern with long‑term Compazine use?
The risk of extrapyramidal symptoms, especially tardive dyskinesia, rises after several weeks of daily use. Doctors usually limit treatment to a few days unless the benefit clearly outweighs the risk.
Is it safe to mix Compazine with other antipsychotics?
Mixing can amplify dopamine blockade, leading to severe sedation or motor side effects. Always get a psychiatrist’s approval before combining any antipsychotic agents.
Which alternative is best for patients who need to stay alert?
Ondansetron or Granisetron are the least sedating options because they target serotonin rather than histamine or dopamine pathways.
Can I take Compazine while pregnant?
Compazine is a Category C drug, meaning animal studies showed some risk and there aren’t enough human studies. Discuss alternatives like Ondansetron (Category B) with your OB‑GYN before deciding.
What should I do if I miss a dose of Compazine?
Take the missed dose as soon as you remember, unless it’s almost time for the next scheduled dose. In that case, skip the missed one-don’t double up.
Are there any food or drink restrictions with Compazine?
Avoid alcohol because both can increase sedation. Caffeine can mask drowsiness, which might lead you to underestimate how sleepy you actually are.
Whether you land on Compazine or one of its alternatives, the right choice hinges on the exact cause of nausea, your tolerance for side‑effects, and any other health conditions you have. Use the comparison table, the decision factors, and the FAQ as a checklist before you or your clinician finalize the prescription.


ahmed ali
October 26, 2025 AT 19:40Compazine blocks dopamine receptors, which means it can quell nausea but also messes with motor pathways.
While the article paints it as a silver bullet, the real world sees a high incidence of extrapyramidal side‑effects, especially when patients are on it for more than a few days.
What many forget is that the drug’s antihistamine and anticholinergic actions add a sedative cloud that can impair cognition, something you can’t afford on a long road trip.
Also, the claim that it’s superior for migraine‑related nausea ignores the fact that metoclopramide offers similar dopaminergic blockade with added pro‑motility benefits.
Cost is another hidden factor; generic compazine can be pricey for uninsured patients compared to off‑label promethazine which is ubiquitous and cheap.
Pharmacologically, its dopamine D2 antagonism is not selective – it also hits D1 receptors, heightening the risk of dystonic reactions.
Clinicians should also be wary of drug‑drug interactions, as compazine can potentiate the QT‑prolonging effects of certain antibiotics, a detail left out in many lay summaries.
In terms of onset, oral dosing takes 30‑60 minutes, but IV administration isn’t always available in urgent care settings, limiting its practicality.
For patients with a history of Parkinson’s or movement disorders, even a single dose can tip the balance toward tremor or rigidity, making alternatives like ondansetron far safer.
The article’s decision tree assumes everyone can tolerate sedation, yet many elderly patients experience falls due to the drug’s dizziness and dry mouth.
Long‑term use is especially problematic; tardive dyskinesia rates climb after just a few weeks of daily dosing, a risk that outweighs the modest anti‑emetic benefit for most chronic conditions.
Moreover, the notion that compazine doubles as an antipsychotic is misleading – the antipsychotic dose is much higher than what you’d prescribe for nausea, so you’re essentially giving a sub‑therapeutic psych dose with unwanted side‑effects.
If you’re looking for a rapid IV anti‑emetic in the ER, other agents like droperidol or even low‑dose haloperidol can achieve similar control without as many movement concerns.
Finally, patient education is crucial: telling someone to “just take it” without warning about muscle stiffness or the need to report any facial twitching does more harm than good.
In short, compazine is a tool with very specific niches, not a universal fix for every vomiting episode.
Deanna Williamson
October 30, 2025 AT 05:53The dopamine blockade in compazine inevitably raises the specter of motor side effects, which many clinicians underplay.
When you compare it head‑to‑head with ondansetron, the movement disorder risk is a clear disadvantage.
Joe Langner
November 2, 2025 AT 17:13Reading through that deep dive reminds us that every medicine is a trade‑off, and the balance between relief and risk is a reflection of the choices we make in our own lives.
Even if compazine feels like a heavy hand, sometimes a firm grip is needed to steady the ship during a storm of nausea.
Just remember, the body often heals itself once the trigger is removed, so using the mildest effective agent is usually the wiser path.
Hope this helps you see the bigger picture and pick what feels right for you.
Katherine Brown
November 6, 2025 AT 04:33In evaluating anti‑emetic options, it is prudent to consider both pharmacodynamic mechanisms and patient‑specific factors such as comorbidities, concomitant therapies, and required level of alertness.
Ondansetron, for instance, demonstrates a favorable side‑effect profile for individuals prone to extrapyramidal symptoms, whereas promethazine may be advantageous when sedation is desired.
Thus, a systematic assessment rather than a singular focus on efficacy alone yields optimal therapeutic decisions.
Tony Stolfa
November 9, 2025 AT 15:53Well, that’s a textbook answer, but let’s be real – most doctors won’t read a paragraph before they just scribble “Compazine” on a prescription pad.
If you want to sound smart, go ahead, but the bedside reality is that time‑pressed clinicians choose the drug they know, even if it’s not the most elegant choice.
Stop polishing it up and just admit the market drives the decision.
Leah Ackerson
November 13, 2025 AT 03:13🤔 Interesting point, though the “market drives the decision” narrative overlooks how insurance formularies dictate availability more than clinician preference.
Still, a dash of nuance never hurts, even for those who love a good drama. 😊
Ramesh Kumar
November 16, 2025 AT 14:33Hey folks, just a quick heads‑up: if you’re considering compazine, make sure to check your other meds for potential QT‑prolongation interactions, especially if you’re on certain antibiotics or anti‑arrhythmics.
Also, the IV form works faster than oral – perfect for emergency rooms.
sarah basarya
November 20, 2025 AT 01:53Oh, look at you dropping the “quick heads‑up” like it’s a spoiler for a blockbuster movie.
Honestly, most patients don’t care about the pharmacology drama; they just want the nausea to stop, and they’ll take whatever you serve.
Samantha Taylor
November 23, 2025 AT 13:13Compazine isn’t the only game in town.
Ben Dover
November 27, 2025 AT 00:33While brevity has its merits, a nuanced discourse reveals that the therapeutic landscape encompasses multiple agents, each with distinct receptor affinities, pharmacokinetics, and safety considerations that warrant thorough examination beyond a mere statement.
Holly Kress
November 30, 2025 AT 11:53Let’s keep the conversation constructive: if you’re new to anti‑emetics, start by matching the drug’s mechanism to the underlying cause of nausea, and then weigh side‑effects against lifestyle needs.
Feel free to ask for clarification on any point you find unclear.
renee granados
December 3, 2025 AT 23:13Sure, but you’ve never heard about the hidden agenda of pharma companies pushing certain anti‑nausea drugs to keep patients dependent on their patented products.