When you start a new medication for pain, depression, or high blood pressure, you expect relief-not a new problem that makes you feel stuck. But for medication-induced constipation, that’s exactly what happens. Up to 60% of people on long-term opioids, and nearly a third of those taking anticholinergics like Benadryl, develop constipation that doesn’t go away with just more fiber or water. This isn’t just uncomfortable-it’s common enough to make people quit life-changing drugs. The good news? There’s a smarter way to handle it, and it starts with knowing why your meds are doing this.
Why Your Medication Is Slowing You Down
Not all constipation is the same. If you’ve ever tried psyllium husk (Metamucil) for constipation from pills and it made things worse, you’re not alone. That’s because most over-the-counter fixes assume your gut is just dry or sluggish. But when drugs cause constipation, they’re attacking your gut’s nervous system directly. Opioids like oxycodone or morphine bind to receptors in your intestines. These receptors normally help move food along. When they’re blocked, your gut slows down. Fluid gets absorbed, stools harden, and your body forgets how to push. The result? Bowel movements drop from daily to once a week or less. Studies show this happens in 40-60% of chronic opioid users. Anticholinergics-found in older allergy meds, sleep aids, and even some antidepressants-do something similar. They block acetylcholine, a key messenger that tells your gut to contract. Without it, your intestines barely move. One study showed a 30-40% drop in gut motility just from taking diphenhydramine. Even common OTC drugs like Benadryl can trigger this. Calcium channel blockers like verapamil relax the muscles in your blood vessels to lower blood pressure. But they also relax the smooth muscle in your colon. That means slower transit time-up to 25% slower. Iron supplements? They cause inflammation in the gut lining and mess with your microbiome, slowing things down by 25-30%. Diuretics? They dehydrate you. Less water in your system means harder stools, and low potassium from these drugs further weakens gut contractions. The real kicker? These drugs don’t just slow things down-they also make your anal sphincter tighter and dull your urge to go. So even if some stool makes it through, you can’t push it out easily.Why Fiber Won’t Fix This
You’ve probably heard: “Eat more fiber. Drink more water.” It’s standard advice for constipation. But for medication-induced constipation, it often backfires. Fiber adds bulk. That’s great if your gut is moving normally. But if your gut is already paralyzed by opioids or anticholinergics, adding bulk just makes you feel bloated and more backed up. In fact, 20-30% of people on opioids report worse symptoms after starting psyllium. One clinical analysis found fiber supplements increased discomfort by 10-15% in MIC patients. Water helps-but only if your gut can still move. If your colon isn’t contracting, drinking 3 liters a day won’t help. That’s why hydration alone is only 20-30% effective for drug-related constipation. It needs to be paired with the right kind of laxative.What Actually Works: Laxatives Matched to the Cause
The key to fixing medication-induced constipation isn’t guessing. It’s matching the treatment to the mechanism. For opioid-induced constipation, the gold standard is a class of drugs called PAMORAs-peripheral μ-opioid receptor antagonists. These include methylnaltrexone (Relistor), naloxegol (Movantik), and naldemedine (Symproic). They block opioids from acting in the gut without touching their pain-relieving effects in the brain. Relistor works in 4-6 hours. In trials, it increased spontaneous bowel movements by 30-40%. That’s not just relief-it’s restoration. If PAMORAs aren’t available or too expensive, the next best option is a combination of osmotic and stimulant laxatives. Polyethylene glycol (PEG 3350, like Miralax) pulls water into the colon. Sennosides (like Senokot) stimulate the nerves that trigger contractions. Together, they work in 60-70% of patients. BC Cancer guidelines recommend starting sennosides (17-34mg daily) on day one of opioid therapy-not after constipation shows up. For anticholinergic-induced constipation, the best fix is often switching meds. If you’re on diphenhydramine for sleep or allergies, try loratadine (Claritin) or cetirizine (Zyrtec). They cause constipation in only 2-3% of users, compared to 15-20% with Benadryl. Same for antidepressants: switch from amitriptyline to a newer SSRI if possible. For calcium channel blockers, verapamil is more likely to cause constipation than amlodipine. If you’re on verapamil and struggling, ask your doctor about switching. For iron supplements, try switching to a slower-release form or taking them every other day. Pair it with vitamin C to help absorption and reduce gut irritation.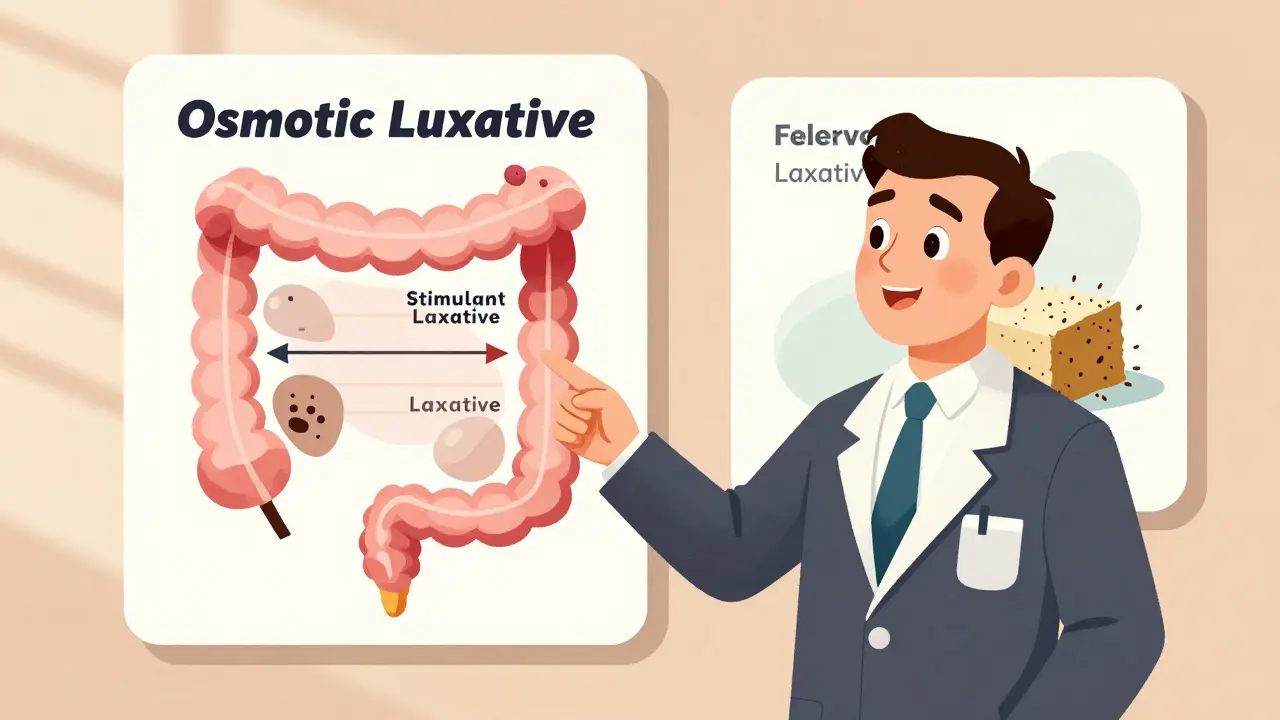
What to Avoid
There are traps everyone falls into. Here’s what to skip:- Waiting until you’re backed up to start treatment. By then, it’s harder to reverse. Prophylaxis works better than rescue.
- Using enemas or suppositories long-term. They’re okay for emergencies, but they train your body to need them. That leads to dependency.
- Overdoing stimulant laxatives. Sennosides are fine daily, but if you’re using them for weeks without improvement, you need a different plan.
- Assuming all laxatives are equal. Dulcolax (bisacodyl) helps some, but doesn’t work as well as PEG + sennosides for opioid users.
Real Stories, Real Results
On Reddit’s r/ChronicPain, 78% of users said they quit opioids-not because the pain returned, but because constipation was unbearable. Only after trying Relistor did they find relief. One user wrote: “Six months of suffering. One injection. I slept through the night for the first time in a year.” In cancer care, patients on clozapine (an antipsychotic) often need daily laxatives. But 40% still report inadequate relief. Those who combine PEG 17g daily with sennosides 17mg report complete prevention of constipation. That’s the kind of precision that works. The downside? Cost. Relistor can run $1,200 a month without insurance. Many patients wait 3+ months to get it approved. But if you’re on long-term opioids and struggling, it’s worth pushing for. Insurance often covers it if you’ve tried and failed with standard laxatives.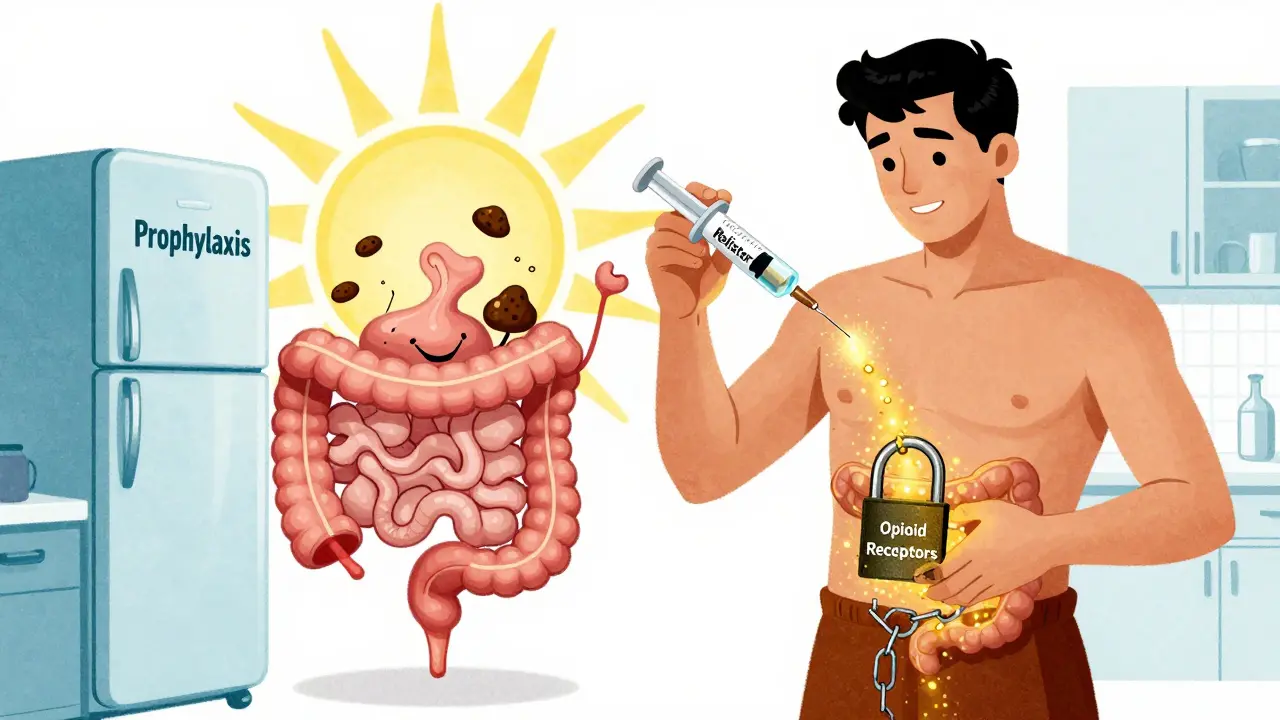
How to Talk to Your Doctor
Most doctors know constipation is common. But many still don’t know how to treat it properly. Only 35-40% of primary care providers follow evidence-based guidelines for MIC. When you bring it up, be specific:- “I started [medication name] and haven’t had a bowel movement in 5 days.”
- “I tried fiber and water, but it made me bloated.”
- “I’ve read that PAMORAs like Relistor work for opioid-induced constipation. Can we talk about that?”
- “Is there a different medication that’s less likely to cause this?”
What’s Coming Next
Research is moving fast. New drugs are being tested that target the gut’s microbiome. Seres Therapeutics’ SER-287, currently in Phase 2 trials, has shown 40-50% improvement in MIC symptoms by restoring healthy bacteria. Mayo Clinic is already using AI in its electronic health records to flag patients at high risk for constipation and auto-prescribe prophylactic laxatives. That system cut MIC cases by 30%. The future is personalized. Not everyone needs the same fix. Your treatment should match your drug, your gut, and your lifestyle.Bottom Line
Medication-induced constipation isn’t a side effect you have to live with. It’s a predictable, treatable problem. You don’t need to suffer. You don’t need to quit your meds. You just need the right tools. Start by identifying which drug is likely causing it. Then match the treatment to the mechanism. Skip the fiber if you’re on opioids. Don’t wait to act. And if your doctor says “just drink more water,” push back. There’s a better way.Can constipation from medication be permanent?
No, medication-induced constipation is not permanent. Once the drug is stopped or the right treatment is started, bowel function usually returns to normal. However, if left untreated for months, chronic straining can lead to complications like hemorrhoids or rectal prolapse. Early intervention prevents long-term damage.
Is it safe to take laxatives every day for medication-induced constipation?
Yes, certain laxatives are safe for daily use when prescribed for medication-induced constipation. Polyethylene glycol (PEG) and sennosides are both approved for long-term use in this context. Unlike stimulant laxatives like senna, which can cause dependency if used improperly, PEG works by drawing water into the colon and doesn’t alter nerve function. Always follow your doctor’s dosage-typically 17g of PEG daily and 17-34mg of sennosides.
Why does my doctor keep telling me to eat more fiber when it makes me worse?
Many doctors still follow outdated advice that fiber helps all constipation. But for medication-induced constipation, especially from opioids or anticholinergics, fiber can make bloating and discomfort worse because your gut can’t move the added bulk. Studies show 20-30% of patients on opioids report increased symptoms after starting psyllium. You’re not wrong to feel worse-you’re just getting the wrong advice. Ask for osmotic or stimulant laxatives instead.
What’s the difference between Relistor and Miralax?
Relistor (methylnaltrexone) is a PAMORA-it blocks opioid receptors in the gut only, without affecting pain relief. It works in 4-6 hours and is used specifically for opioid-induced constipation. Miralax (PEG) is an osmotic laxative that pulls water into the colon to soften stool. It works in 1-3 days and is used for general constipation. For drug-induced cases, Miralax helps, but Relistor targets the root cause. Many patients use both: Relistor for fast relief, Miralax for daily maintenance.
Are there any natural remedies that work for medication-induced constipation?
Natural remedies like prunes, flaxseed, or probiotics have limited effect on medication-induced constipation. They may help a little if your gut still has some movement, but they won’t overcome the nerve-blocking effects of opioids or anticholinergics. A 2023 study showed that even high-dose probiotics improved symptoms in only 15-20% of MIC patients. For real relief, you need targeted medications like PEG, sennosides, or PAMORAs.
How long should I wait before calling my doctor about constipation from a new medication?
Don’t wait. If you haven’t had a bowel movement in 3 days after starting a new medication, contact your doctor. For high-risk drugs like opioids or anticholinergics, guidelines recommend starting a laxative on day one. Waiting until you’re in pain or bloated means you’re already behind. Early action prevents complications and keeps you on your essential meds.


Tim Bartik
December 15, 2025 AT 14:09bro i was on oxycodone for 2 years and tried EVERYTHING-psyllium, prunes, enemas, even that weird yoga pose my cousin swears by. nothing. then i found out about Relistor. one shot and i felt like a human again. my wife cried. i cried. we both cried. worth every damn penny even if insurance fights you. fuck fiber, it just made me feel like a balloon filled with bricks.
Daniel Thompson
December 16, 2025 AT 08:20While the article presents a compelling clinical perspective on medication-induced constipation, it is imperative to acknowledge the methodological limitations inherent in self-reported data from online forums such as Reddit. The generalizability of anecdotal evidence, particularly when correlated with pharmaceutical efficacy, remains statistically questionable without controlled longitudinal studies. Furthermore, the assertion that fiber exacerbates symptoms lacks a robust meta-analytical foundation.
Alexis Wright
December 16, 2025 AT 14:47Let’s be real-this isn’t about constipation. It’s about the pharmaceutical-industrial complex keeping you docile. Opioids? They’re not just blocking your gut-they’re blocking your autonomy. PAMORAs? A Band-Aid on a bullet wound. They don’t want you to know you can wean off opioids entirely. They want you hooked on the solution, not the cure. And don’t get me started on how the FDA approves drugs that wreck your bowels but never the ones that fix them. Wake up. This is control. And Miralax? It’s the sugar coating on the poison pill.
Natalie Koeber
December 18, 2025 AT 11:48okay but what if the gov is secretly adding fluoride to the water to slow down our digestion so we don't move around too much?? like... why do you think all these meds cause constipation? it's not an accident. they want us sedated. and the 'doctors' are in on it. i read this one blog that said the same people who make benadryl also make the chips you eat at the movies. it's all connected. 🤫👁️
Wade Mercer
December 18, 2025 AT 17:08People who quit their meds because of constipation are just giving up too easily. Suffering builds character. If you can't handle a little discomfort, how are you supposed to handle life? I’ve been on verapamil for 12 years and I’ve only had one bowel movement in the last week. I’m proud of that. It’s a test of willpower.
Dwayne hiers
December 19, 2025 AT 17:16Important clarification: PEG 3350 is osmotic, non-absorbable, and does not alter colonic motility-making it ideal for long-term use in MIC. Sennosides act as stimulant laxatives via anthraquinone derivatives, enhancing propulsive contractions. For opioid-induced cases, PAMORAs are first-line per AGA guidelines (2022), but PEG + sennosides combo achieves >65% efficacy in real-world cohorts. Avoid bisacodyl in chronic use due to potential enteric neuropathy. Always monitor electrolytes with diuretic-induced MIC. Prophylaxis > rescue.
Jonny Moran
December 20, 2025 AT 00:29Hey everyone, I’ve been where you are. Took me 18 months to figure this out, but I’m back to hiking, sleeping through the night, and not dreading breakfast. You’re not broken. You’re just on the wrong treatment plan. Don’t let a doctor who says ‘just drink water’ make you feel crazy. You’re smart for reading this. Keep pushing. You deserve to feel normal again. I believe in you. 💪
Sarthak Jain
December 21, 2025 AT 20:40bro i was on amitriptyline for anxiety and my gut just… stopped. i switched to sertraline and boom, 3 days later i had a normal BM. no laxatives. no injections. just a med swap. also, probiotics helped a lil, but not like the article says. maybe it was the sleep i got after not being bloated? idk. but yeah, talk to your doc about switching. it’s not always about laxatives. 🙏
Sinéad Griffin
December 23, 2025 AT 10:38THIS. IS. LIFE. 🥹💖 I was on morphine for 3 years and thought I’d never poop again. Then I got Relistor. Now I’m back to baking pies, going to concerts, and not crying in the bathroom. Thank you for writing this. I’m sharing it with my entire family. You saved my life. 🌟