Fentanyl Patch Heat Risk Checker
This tool helps you understand how heat exposure affects your fentanyl patch risk. Based on FDA and medical guidelines, it assesses your current situation for potential overdose danger.
It’s not just about taking the patch as prescribed. If you’re using a fentanyl patch for chronic pain, and you turn up the heat - whether it’s a heating pad, a hot shower, or even a fever - you could be putting your life at risk. Fentanyl patches are designed to release a steady, controlled dose of opioid over three days. But heat doesn’t just make you feel warmer. It can trigger a dangerous surge in drug absorption, leading to overdose - even if you’ve been using the patch for months without issue.
How Fentanyl Patches Work (And Why Heat Changes Everything)
Fentanyl patches, like Duragesic, aren’t like swallowing a pill. They’re sticky, adhesive patches that slowly push fentanyl through your skin and into your bloodstream. The system is engineered to release about 25 micrograms per hour over 72 hours. That’s precise. That’s intentional. And that’s why heat breaks the system.
When your skin warms up - say, from a heating pad set to 40°C (104°F) - the blood vessels under the patch dilate. More blood flows through the area. The fentanyl, which was meant to trickle out slowly, now gets pulled into your bloodstream faster. Studies show this can increase blood levels of fentanyl by up to 33%. In one controlled experiment, researchers used a special heat patch over a fentanyl patch and saw serum concentrations nearly triple. That’s not a small bump. That’s a leap into overdose territory.
Even without external heat sources, your body can create the same danger. A fever, intense exercise, or lying under a warm blanket after surgery can all raise skin temperature enough to speed up absorption. And here’s the scary part: you might not feel it coming. No warning signs. No sudden pain. Just slow, silent respiratory depression - your breathing gets shallow, then stops. That’s how people die from fentanyl patches when they didn’t take more than prescribed.
What Heat Sources Are Actually Dangerous?
It’s not just the obvious ones. Yes, heating pads and electric blankets are clear risks. But so are:
- Saunas and steam rooms
- Hot tubs and long, steamy showers
- Sunbathing or prolonged exposure to direct sunlight
- Heated car seats or massage chairs
- Warming blankets used during surgery or hospital stays
- Even wearing tight clothing that traps body heat over the patch site
One documented case involved a patient who developed a fever after surgery. He was on a fentanyl patch for cancer pain. His body temperature hit 39.5°C. He stopped breathing. He didn’t survive. Another patient used a heating pad for back pain - same patch, same dose - and collapsed from respiratory failure. These aren’t rare accidents. They’re predictable outcomes of ignoring basic safety rules.
And here’s something many people don’t realize: the patch continues to release fentanyl for hours after you take it off. That’s because the drug sits in your skin like a reservoir. If you use heat right after removing the patch - say, you take it off before bed and then turn on a heating pad - you’re still at risk. The fentanyl is still there, still moving into your blood.
Who Should Never Use Fentanyl Patches?
Fentanyl patches are not for everyone. They are strictly for people who are already tolerant to opioids - meaning they’ve been taking regular opioid painkillers for a while and their body has adapted. They are NOT for:
- People taking opioids for the first time
- Patients with acute pain, like after surgery or an injury
- Anyone under 18, unless under strict specialist supervision
- People with breathing problems like sleep apnea or COPD
Why? Because a single patch can deliver a lethal dose to someone who hasn’t built up opioid tolerance. A 25 mcg/hour patch contains enough fentanyl to kill an opioid-naïve person in minutes. That’s why doctors require proof of prior opioid use before prescribing them. But even if you’re tolerant, heat can turn a safe dose into a deadly one.

What to Do If You’re Already Using a Fentanyl Patch
If you’re on a fentanyl patch, here’s what you need to do right now:
- Never use heat directly over the patch. That includes heating pads, warm compresses, or even hot water bottles.
- Avoid saunas, hot tubs, and long hot showers. Keep water warm, not scalding.
- Check your temperature if you feel sick. A fever can increase absorption. Call your doctor immediately if your temperature rises above 38°C (100.4°F).
- Don’t sunbathe. Even sitting in the sun for hours can raise skin temperature enough to be risky.
- Remove the patch exactly 72 hours after applying it. Don’t leave it on longer. Don’t cut it. Don’t reuse it.
- Watch for signs of overdose: extreme drowsiness, slow or shallow breathing, cold/clammy skin, confusion, unresponsiveness.
If you notice any of those signs - call 911 immediately. Don’t wait. Naloxone (Narcan) can reverse opioid overdose, but it must be given fast. And if you’re on a fentanyl patch, you might need multiple doses.
Other Medications That Make It Worse
Heat isn’t the only danger. Some common drugs can also raise fentanyl levels dangerously:
- Antibiotics like erythromycin
- Antifungals like ketoconazole
- Some antidepressants and antivirals
These drugs block the liver enzyme (CYP3A4) that breaks down fentanyl. So even if you’re not using heat, your body can’t clear the drug properly. The result? Higher blood levels. Same risk. Same danger.
Always tell your pharmacist and doctor about every medication you take - even over-the-counter ones. They need to check for interactions. One wrong combo can be fatal.
What About Other Opioid Patches?
Not all patches are the same. Buprenorphine patches (like Butrans) are less sensitive to heat. But fentanyl? It’s one of the most dangerous. That’s why the FDA and Mayo Clinic have issued repeated warnings. The risk isn’t theoretical. It’s been proven in real patients. In one study, three people died from fentanyl overdose after heat exposure - one from a heating pad, one from a surgical warming blanket, and one from intense physical activity.
If you’re worried about your current patch, talk to your doctor. There are alternatives: extended-release pills, different pain management strategies, or even non-opioid treatments. You don’t have to stick with something that puts you at risk.
What to Do After a Patch Is Removed
Even after you take off the patch, don’t assume it’s safe. Fentanyl stays in your skin for hours - sometimes up to 24 hours. So:
- Don’t use a heating pad right after removal
- Avoid hot baths or saunas for at least a full day
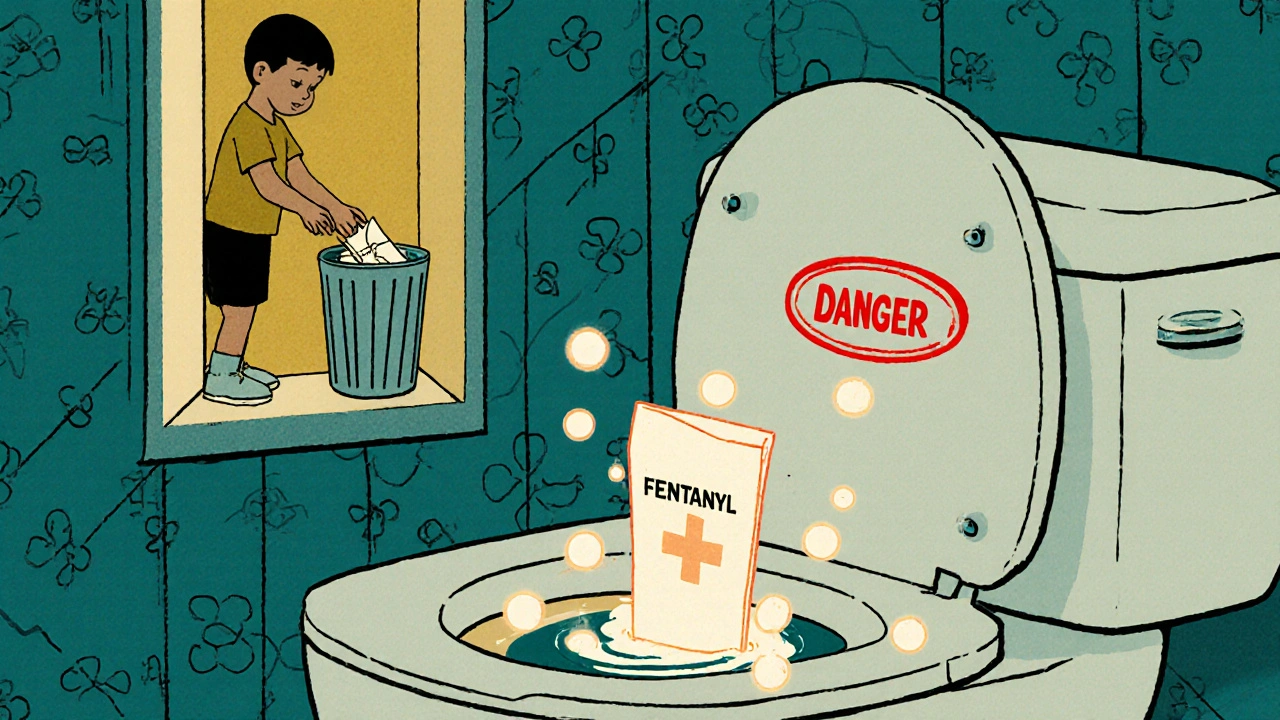
- Keep the used patch folded in half (sticky side in) and flush it down the toilet or return it to your pharmacy
Never throw it in the trash where someone else - a child, a pet - could find it. One patch can kill.
Can I use a fentanyl patch if I have a fever?
No. A fever raises your body temperature, which can cause the patch to release fentanyl faster. This increases the risk of overdose. If you develop a fever while using a fentanyl patch, contact your doctor immediately. Do not wait for symptoms to appear.
What happens if I accidentally expose my patch to heat?
If you use a heating pad, take a hot shower, or get a fever while wearing the patch, remove it immediately and call your doctor. Watch for signs of overdose: slow breathing, extreme drowsiness, confusion, or unresponsiveness. If these occur, call 911 and give naloxone if available. Don’t assume you’re safe just because you feel fine - overdose can happen without warning.
Are there safer alternatives to fentanyl patches?
Yes. Depending on your condition, your doctor may recommend extended-release oral opioids, non-opioid pain relievers like gabapentin or duloxetine, physical therapy, nerve blocks, or even spinal cord stimulators. Fentanyl patches carry high risks, especially with heat exposure. Ask your doctor if another option could work for you.
Can I use a fentanyl patch after surgery?
No. Fentanyl patches are not approved for acute pain like after surgery. They’re meant for chronic, around-the-clock pain in opioid-tolerant patients. Using them after surgery - especially with warming blankets - can cause a fatal overdose. Always tell your surgical team if you’re on a fentanyl patch.
How do I safely dispose of a used fentanyl patch?
Fold the patch in half so the sticky sides stick together. Flush it down the toilet immediately. Do not throw it in the trash. Even a used patch still contains enough fentanyl to kill a child or pet. Some pharmacies offer take-back programs - ask yours. Never leave used patches where others can find them.


Brierly Davis
November 7, 2025 AT 19:47Just got my first fentanyl patch last week for chronic back pain. This post literally saved my life. I was about to use my heating pad like usual-thank god I scrolled past this. I’m telling my whole family about this. Don’t be like me and assume it’s fine. Heat + patch = bad news. 🙏
Jim Oliver
November 9, 2025 AT 08:38Of course people die. They treat opioids like candy. You don’t get to ignore physics because you’re ‘used to it.’ Heat increases kinetic energy-duh. Blood flow increases. Drug absorption spikes. It’s not magic. It’s chemistry. And yet, here we are. People die because they think their ‘experience’ makes them immune. It doesn’t.
William Priest
November 10, 2025 AT 22:05fr tho, fentanyl patches are like a russian roulette with a 3 day timer. you think ur cool cuz u been on em for years? bro, ur skin’s a sponge now. heat? lol. even your damn sweat can do it. i saw a dude pass out in a hot tub after his patch. he was 52. had a 100mcg/hr one. dead in 20 mins. no warning. just… gone. smh.
Ryan Masuga
November 12, 2025 AT 15:24Hey, I know this sounds scary-but you’re not alone. If you’re on a patch, you’re already doing the hard work of managing pain. This info isn’t meant to scare you off treatment-it’s meant to help you stay safe. Talk to your doc about alternatives if you’re worried. There are options. You deserve relief without risking your life. You got this 💪
Jennifer Bedrosian
November 14, 2025 AT 13:48OMG I just realized I’ve been taking hot showers with my patch on for 2 years 😭 I thought it was fine because I didn’t feel anything. I just yanked it off and called my doctor. I’m so scared right now. What if I already did damage? I feel like such an idiot. But thank you for posting this. I’m sharing it with everyone I know.
Lashonda Rene
November 15, 2025 AT 18:16I’ve been on these patches for 7 years and I never knew that even after you take it off it’s still in your skin. I used to take the patch off at night and then go to bed under a heated blanket because my hands get cold. I had no idea I was still getting hit with the drug. I just thought I was being cozy. Now I’m terrified. I’m going to stop using blankets over the area and I’m telling my mom too. She’s on one too. I just didn’t know. No one told me. This needs to be on every prescription label.
Andy Slack
November 17, 2025 AT 01:54My dad’s on a fentanyl patch for cancer pain. I’m printing this out and taping it to his bathroom mirror. No more hot tubs. No more heating pads. No more ‘just a little warmth.’ He’s my hero. He’s fighting hard. He doesn’t need to lose this battle to a stupid mistake. Thanks for the clarity.
Rashmi Mohapatra
November 17, 2025 AT 05:45Why are you even using patches? In India we just take pills. Much safer. You Americans love your fancy tech but you ignore the basics. Heat? Who cares? Just don’t use it. Simple. You make it sound like magic. It’s just science. You people overthink everything.
Abigail Chrisma
November 18, 2025 AT 05:46Thank you for sharing this so clearly. I’m a nurse in rural Maine, and I’ve seen too many patients assume their patch is ‘safe’ because they’ve used it for years. One woman came in after her grandson found her used patch in the trash-she didn’t know it could kill a child. We need more posts like this. I’m printing copies for my clinic. And to everyone on here: if you’re scared, you’re not weak. You’re awake. That’s the first step to staying alive.