When you’re 70, your body doesn’t process medicine the same way it did at 30. That’s not just a myth-it’s science. Older adults are more than twice as likely to have serious side effects from medications than younger people. And it’s not because they’re taking too many pills-it’s because their bodies have changed. The same dose that helped someone at 50 might send a 75-year-old to the hospital. This isn’t rare. About 35% of hospital stays for people over 65 are caused by medications that didn’t work the way they were supposed to. And half of those could have been avoided.
Why Your Body Changes How It Handles Medicine
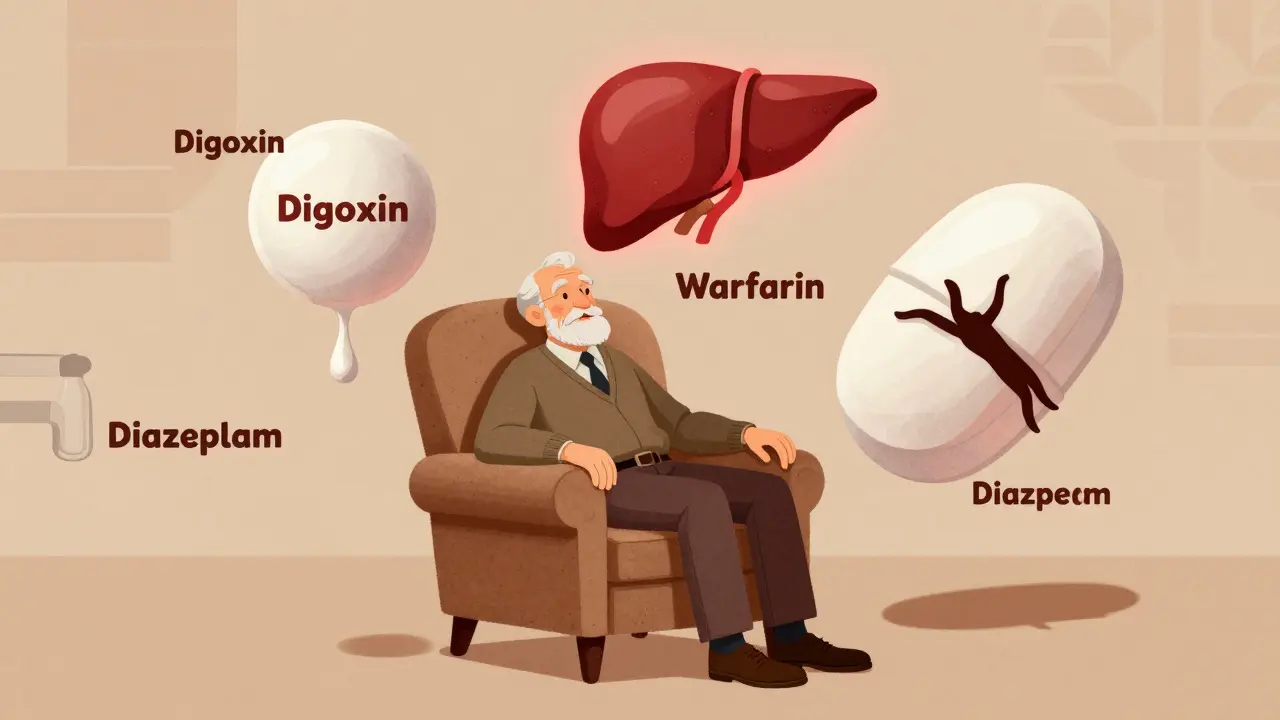
As you age, your body’s chemistry shifts in ways that directly affect how drugs move through you. Think of it like an old car engine: the same fuel might work fine when it’s new, but over time, the parts wear down and need adjustment. Your kidneys, which filter out most drugs, lose about 30-50% of their function between ages 30 and 80. That means drugs like digoxin, antibiotics, and painkillers stick around longer in your system. If your dose hasn’t been lowered, you’re essentially overdosing slowly. Your liver, which breaks down many medications, also slows down. Blood flow to the liver drops by 20-40% after age 65. That affects drugs like propranolol and verapamil, which rely on liver processing. The result? Higher drug levels in your blood, even if you’re taking the same pill as you did ten years ago. Then there’s body composition. Between ages 25 and 80, total body water drops by 15%, while body fat increases from 25% to nearly 50% in women. That changes how drugs spread through your body. Water-soluble drugs like lithium become more concentrated. Fat-soluble drugs like diazepam build up in fat tissue and release slowly, leading to prolonged sedation. Even your blood changes. Albumin, the protein that binds many drugs, drops by 10-15% in older adults. That means more of the drug is floating around unattached-and active. Warfarin, for example, becomes far more potent. A dose that was safe at 60 can cause dangerous bleeding at 80.How Your Brain and Heart React Differently
It’s not just about how your body handles drugs-it’s about how your organs respond to them. Your brain becomes more sensitive. A 2023 study showed that older adults get 50% more sedation and memory problems from diazepam than younger people, even with the same blood levels. That’s why benzodiazepines like lorazepam or zolpidem are on the Beers Criteria list of medications to avoid in older adults. They don’t just make you drowsy-they cause confusion, falls, and even delirium. Your heart changes too. Beta-blockers like propranolol need 50% higher doses in younger people to get the same effect. But in older adults, the heart doesn’t respond as strongly. So doctors sometimes increase the dose, not realizing that the brain and kidneys are already overloaded. The result? Dizziness, low blood pressure, fainting. Antihypertensives are a big problem. A 2022 study found that 28% of people over 80 had symptoms of low blood pressure-dizziness, falls, weakness-after taking standard doses. Only 9% of people aged 50-65 had the same issue. That’s why so many older adults end up in the ER after a fall: it’s not just balance. It’s medicine.Common Medications That Become Riskier With Age
Some drugs are fine for younger people but dangerous for older adults. The American Geriatrics Society updates the Beers Criteria every two years to flag these. The 2023 list includes 56 medications to avoid or use with extreme caution.- Anticholinergics like diphenhydramine (Benadryl) and oxybutynin: These cause confusion, memory loss, and urinary retention. One study found they increase delirium risk by 4.2 times in people over 75.
- Benzodiazepines like lorazepam and alprazolam: Linked to 2-3 times higher risk of falls and hip fractures. Zolpidem causes 80% more next-day drowsiness in people over 65.
- NSAIDs like ibuprofen and naproxen: Increase risk of stomach bleeding and kidney damage. In older adults, even short-term use can cause acute kidney failure.
- Antidepressants like amitriptyline: Cause urinary retention in men with enlarged prostates and severe dry mouth. One Reddit user at 78 was catheterized within days of starting it.
- Warfarin: Requires 20-30% lower doses in older adults. INR levels become unstable in 35% of seniors, compared to 15% in younger people.
Polypharmacy: When More Pills Mean More Danger
Forty-eight percent of adults over 65 take five or more prescription drugs every month. That’s called polypharmacy. And it’s not just about the drugs themselves-it’s about how they interact. Take a typical 80-year-old: one pill for blood pressure, another for cholesterol, a third for arthritis, a fourth for sleep, a fifth for anxiety, and maybe a sixth for heart rhythm. Each one has its own side effects. But when you stack them, the risks multiply. A 2022 JAMA study found that people on five or more medications had a 50% higher chance of a serious adverse reaction. And it’s not just prescriptions. Over-the-counter meds, supplements, and herbal products add to the mix. One “Brown Bag Review”-where a pharmacist looks at everything you’re taking-found an average of 3.2 medication errors per patient.What Doctors Should Be Doing (But Often Aren’t)
The solution isn’t to stop all meds. It’s to personalize them. Experts like Dr. Michael Steinman from UCSF say: “Start low and go slow.” That means beginning with 25-50% of the standard adult dose for older patients. But many doctors still prescribe the same dose they’ve used for decades. They also need to ask: “Is this still helping?” That’s called deprescribing. A 2023 study found that 30-50% of medications in nursing homes are unnecessary. Some were started years ago for a condition that’s since improved-or even disappeared. The STOPP/START criteria help doctors decide what to stop and what to start. STOPP identifies harmful prescriptions. START identifies missing ones-like vaccines or bone-strengthening drugs that older adults often don’t get. Every hospital admission for someone over 65 should include a full medication review. Yet, only 30% of hospitals do this consistently. And most primary care visits are 15 minutes long. There’s no time to untangle a 10-pill regimen.What You Can Do to Stay Safe
You don’t have to wait for your doctor to fix this. Here’s what you can do right now:- Bring all your meds to every appointment-including vitamins, supplements, and OTC drugs. Use a pill organizer or take a photo of your medicine cabinet.
- Ask: “Why am I taking this?” and “Is there a safer alternative?”
- Check your kidney function. Ask for an eGFR test-not just a creatinine level. It’s more accurate.
- Watch for new symptoms. Dizziness, confusion, constipation, or sudden weight loss? These aren’t normal aging. They could be side effects.
- Use the Beers Criteria app. It’s free, updated yearly, and available to anyone. Over 125,000 people have downloaded it.

The Bigger Picture: Why This Matters
The U.S. spends $30 billion a year treating preventable drug reactions in older adults. That’s 15% of all medication costs for this group. And it’s only going to get worse. By 2040, nearly one in five Americans will be over 65. New tools are emerging. Pharmacogenomic testing-checking your genes to see how you metabolize drugs-is now being used in clinics. One study found it cut adverse reactions by 35% in older adults on antidepressants. Artificial intelligence tools like MedAware are now used in hospitals to flag dangerous drug combinations. They’ve reduced errors by 42%. But the real change will come when doctors stop treating 80-year-olds like 40-year-olds. When they stop assuming one size fits all. When they start asking: “What does this person need now-not what they needed ten years ago?”Frequently Asked Questions
Why do older adults have more side effects from the same dose of medicine?
As people age, their kidneys and liver work slower, so drugs stay in the body longer. Body fat increases and water decreases, changing how drugs spread. The brain and heart also become more sensitive to certain drugs. Even if the dose is the same, the effect is stronger-and more dangerous.
Is it safe to stop taking a medication if I think it’s causing side effects?
Never stop a medication on your own. Some drugs, like blood pressure or seizure meds, can cause serious withdrawal effects. Instead, talk to your doctor or pharmacist. Keep a symptom journal: when the side effect started, what you were taking, and how bad it was. That helps them decide if it’s the drug or something else.
What is the Beers Criteria, and should I ask my doctor about it?
The Beers Criteria is a list of medications that are potentially risky for older adults, updated every two years by the American Geriatrics Society. It includes drugs that increase fall risk, confusion, kidney damage, or other serious side effects. You should ask your doctor if any of your medications are on the list-and whether there’s a safer option.
Can I still take over-the-counter meds like Benadryl or ibuprofen as I get older?
Benadryl (diphenhydramine) is on the Beers Criteria list because it causes confusion and memory problems in older adults. Ibuprofen and other NSAIDs can damage kidneys and cause stomach bleeding. Even occasional use can be risky. Ask your doctor for alternatives like acetaminophen for pain or non-medication options for allergies.
How often should older adults have their medications reviewed?
At least once a year, but every 3-6 months if you’re taking five or more medications. Every hospital stay, ER visit, or new diagnosis is also a good time to review your whole list. Pharmacists can do a "Brown Bag Review"-where you bring all your pills, and they check for duplicates, interactions, and unnecessary drugs.
Next Steps
If you or someone you care for is over 65 and taking multiple medications:- Write down every pill, vitamin, and supplement you take.
- Schedule a medication review with your doctor or pharmacist.
- Ask: "Is this still necessary? Can we try lowering the dose? Is there a safer option?"
- Watch for dizziness, confusion, falls, constipation, or weight loss-and report them immediately.
- Download the free Beers Criteria app from the American Geriatrics Society.

Eric Gebeke
January 18, 2026 AT 17:52Of course the system’s broken. Everyone knows doctors just prescribe like they’re on autopilot. I’ve seen my dad on 12 pills at 79-half of them were for side effects from the other half. And no one ever asks if he actually needs them. It’s not medicine, it’s corporate profit disguised as care. They don’t care if you fall, as long as the prescription keeps rolling.
And don’t get me started on those ‘Beers Criteria’ apps-useless unless your doctor actually reads them. Most of them still think ‘elderly’ means ‘just slow down’ instead of ‘your body is a different machine now.’
Andrew McLarren
January 19, 2026 AT 12:52While I appreciate the thoroughness of this analysis, I must emphasize the importance of evidence-based clinical judgment in geriatric pharmacotherapy. The physiological changes you describe are well-documented in peer-reviewed literature, particularly in the Journal of the American Geriatrics Society. However, individual variability remains significant, and blanket recommendations may inadvertently overlook patients who benefit from standard dosing regimens.
It is imperative that deprescribing initiatives be implemented within a framework of comprehensive geriatric assessment, rather than as a checklist-driven exercise. The ethical obligation to avoid harm must be balanced with the duty to preserve therapeutic benefit.
Andrew Short
January 19, 2026 AT 16:24Let’s cut the fluff. This isn’t about science-it’s about lazy doctors and pill-pushing pharmacies. Your grandma’s on warfarin because her cardiologist didn’t bother to check her INR in six months. She’s on Benadryl for allergies because the nurse said ‘it’s fine.’ She’s on ibuprofen because ‘it’s just a little pain.’
And now she’s in the ER with a bleed and a fractured hip. This is preventable. It’s not ‘aging.’ It’s negligence. Every single one of those 35% hospitalizations? A failure. Not a tragedy. A failure. And if you’re not screaming about it, you’re part of the problem.
Aysha Siera
January 21, 2026 AT 14:11Robert Davis
January 22, 2026 AT 18:36I’ve read this entire piece three times. And I have to say-there’s something deeply unsettling about how we’ve normalized this. We don’t just accept that older people get sicker from meds-we expect it. We shrug. ‘Oh, that’s just what happens when you get old.’
But what if the problem isn’t aging? What if the problem is that we keep treating 80-year-olds like 40-year-olds with a few extra wrinkles? The system isn’t broken. It’s designed this way. And the worst part? We’re all complicit.
Joni O
January 23, 2026 AT 19:48Y’all need to read this if you’re caring for an older parent or loved one. I did a brown bag review with my pharmacist last month and we cut 4 meds my mom didn’t even remember taking. One was for a UTI from 2018. FOUR.
She’s slept better, stopped stumbling, and even started gardening again. It’s not magic-it’s just paying attention. Ask your doc: ‘Is this still helping?’ And if they look confused? Bring this article. You’ve got power here.
And yes, the Beers app is free. Download it. It’s like a cheat code for staying safe.
Ryan Otto
January 25, 2026 AT 16:03It is curious how Western medicine continues to operate under the assumption that biological aging is a pathology to be managed with pharmacological intervention rather than a natural, inevitable process requiring contextual adaptation. The Beers Criteria, while well-intentioned, represents a technocratic overreach-a quantification of human frailty that reduces complex physiological decline to a checklist of prohibited substances.
One must question whether the real crisis lies not in polypharmacy, but in the cultural infantilization of the elderly, wherein autonomy is systematically eroded under the guise of safety. The solution is not more algorithms, but a reclamation of dignity.
Max Sinclair
January 27, 2026 AT 11:00This is the kind of post that should be required reading for every family with an aging parent. I shared it with my sister after our mom had a fall last year-turns out her sleep med was making her dizzy. We lowered the dose and she’s been fine since.
Just a reminder: if your doctor says ‘it’s fine’ but you feel off, trust yourself. You know your body better than anyone. And if they don’t have time to talk? Find a geriatric pharmacist. They’re like the secret weapon nobody tells you about.
Nishant Sonuley
January 29, 2026 AT 04:56Let’s be real-this whole thing is a symptom of a culture that treats aging like a bug to be patched, not a stage of life to be honored. We’ve turned elders into walking prescription pads. We don’t sit with them. We don’t listen. We just slap on another pill when they start forgetting names or tripping on stairs.
Meanwhile, the real solution? More walks in the park. More home-cooked meals. More human connection. Less polypharmacy. Less ‘doctor, fix me.’ More ‘I’m here with you.’
And yeah, I know-I sound like a hippie. But guess what? The data backs me up. Social isolation kills faster than ibuprofen.
Emma #########
January 30, 2026 AT 09:08I’ve been a nurse for 22 years and I’ve seen this over and over. A woman in her 80s comes in with confusion and falls. Family says she’s ‘just getting old.’ We pull her meds-turns out she’s on three anticholinergics, a benzo, and a beta-blocker. All started by different doctors.
One week after we tapered them? She’s laughing again. Recognizes her grandkids. Walks without a cane.
This isn’t magic. It’s just stopping the harm. Please, if you’re reading this-ask for a med review. Don’t wait for a crisis.
Danny Gray
January 31, 2026 AT 05:51Interesting. But what if the real issue isn’t the drugs-but the fact that we’re forcing people to live longer than their bodies are meant to? We’re medicating decline instead of accepting it. What if the body knows when to stop? What if we’re just prolonging suffering with a pill?
I’m not saying don’t treat illness. But we’ve turned medicine into a weapon against mortality itself. And in doing so, we’ve lost the art of dying well.
Maybe the most dangerous drug isn’t on the Beers list-it’s the belief that we can outsmart death with a prescription.