Head Injury & Nocturia Risk Calculator
This tool estimates your risk of experiencing nocturia (waking up multiple times at night to urinate) after a head injury. Please answer the following questions about your situation.
Risk Assessment Results
Key Takeaways
- Head injuries can disrupt the brain circuits that control bladder function, often causing nocturia.
- Hormonal changes, especially reduced antidiuretic hormone (ADH), are a common physiological link.
- Cognitive impairment and sleep‑disordered breathing after injury worsen nighttime urination.
- Proper assessment includes neurological exam, sleep study, and bladder diary.
- Treatment blends medication management, bladder training, and rehab for the underlying brain injury.
Ever woken up multiple times at night to pee after a concussion or more serious brain injury? You’re not imagining it. head injuries and nocturia share a surprisingly direct connection that many doctors still overlook. This article walks you through why the link exists, how to pinpoint the cause, and what practical steps can restore a normal night’s sleep.
First, let’s define the two main players.
Head injury is a damage to the skull or brain caused by impact, acceleration, or penetration. It ranges from mild concussions to severe traumatic brain injury (TBI).
Nocturia is the condition of waking one or more times during the night to urinate, interrupting sleep. It is a symptom, not a disease, and can stem from many systems-including the urinary tract, cardiovascular system, and central nervous system.
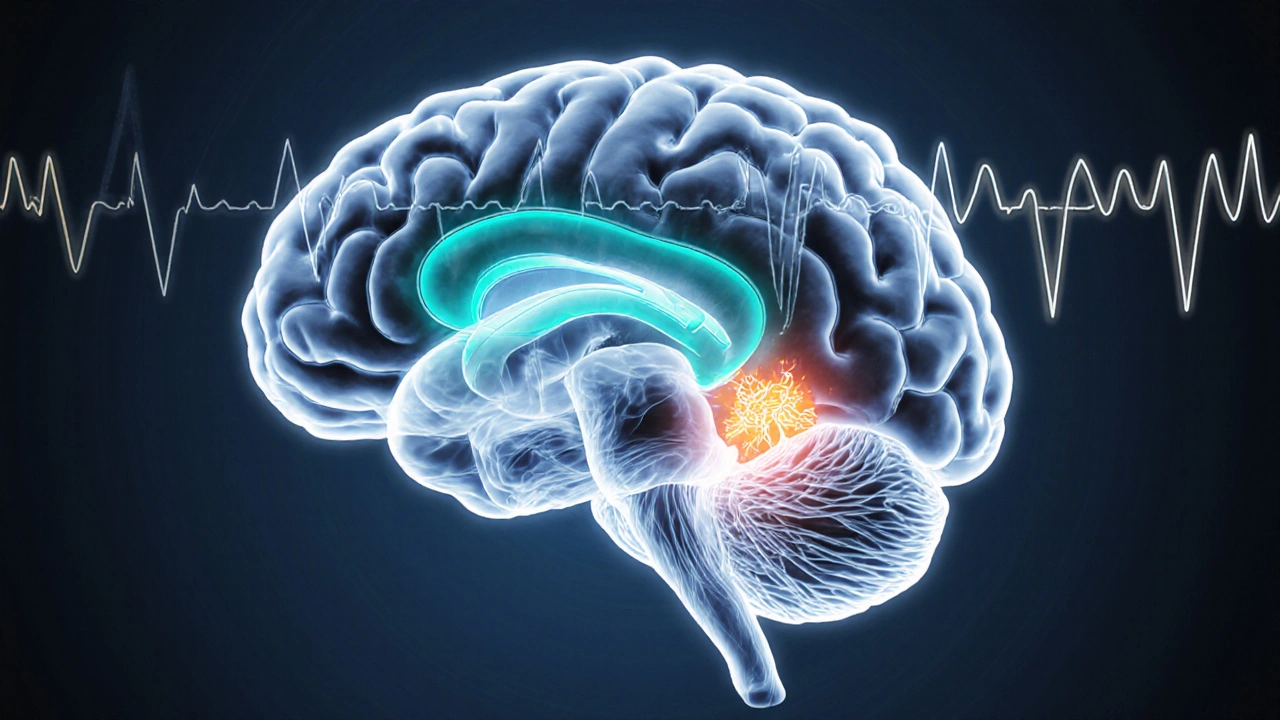
Why the Brain Controls Your Bladder at Night
The brain’s bladder‑control center sits in the pontine micturition center (PMC), coordinating signals from the bladder wall, spinal cord, and higher cortical areas. When the PMC gets mixed messages, the body either holds urine longer or empties it too early. After a head injury, several pathways get disrupted:
- Hormonal shift: The hypothalamus regulates antidiuretic hormone (ADH). Injury can blunt ADH release, leading to more urine production at night.
- Neurogenic bladder: Damage to the PMC or its connections creates an “overactive” bladder that fires during sleep.
- Cognitive and sleep interference: Post‑injury fatigue, memory lapses, or sleep‑disordered breathing make it harder to stay asleep, so the urge to pee feels louder.
Let’s unpack each of these mechanisms.
1. Antidiuretic Hormone (ADH) Disruption
Antidiuretic hormone (also called vasopressin) is a peptide hormone that tells the kidneys to re‑absorb water, reducing urine volume. After a traumatic brain event, the hypothalamus may produce less ADH, especially during the evening. The result? The kidneys dump more fluid when you’re supposed to be sleeping, prompting multiple bathroom trips.
2. Neurogenic Bladder from Direct Brain Damage
Neurogenic bladder is a dysfunction of bladder control caused by nervous system injury. When the brain can’t correctly signal the bladder’s sphincter muscles, the bladder contracts inappropriately. This often shows up as urgency and nocturia rather than daytime frequency alone.
3. Sleep‑Disordered Breathing and Cognitive Load
Sleep apnea, a common companion after head trauma, lowers oxygen levels and triggers nighttime awakenings. Each awakening resets the bladder‑urge threshold, making you more likely to notice the need to void. Additionally, cognitive impairments can reduce the ability to suppress the urge until morning.
Other Factors That Mimic or Amplify the Link
Not every night‑time bathroom break after a head injury is directly caused by the brain. Several co‑existing conditions can either mask the true source or worsen nocturia.
| Contributor | Primary Mechanism | Key Red Flags |
|---|---|---|
| Head injury (TBI) | ADH reduction, neurogenic bladder, sleep disruption | Recent concussion, memory loss, balance issues |
| Prostate enlargement | Urinary outflow obstruction | Weak stream, hesitancy, daytime frequency |
| Diabetes mellitus | Hyperglycemia‑induced polyuria | High blood sugar readings, dry mouth |
| Sleep apnea | Frequent arousals, hormonal imbalance | Snoring, witnessed pauses, morning headache |
| Medication side effects | Diuretics, anticholinergics, sedatives | New prescription, dosage change |
How to Diagnose the Brain‑Related Component
When a patient reports nocturia after a head injury, a focused work‑up can separate neurological causes from more routine ones.
- Detailed history: Note the timing of the injury, any loss of consciousness, current medications, and sleep patterns.
- Bladder diary: Record fluid intake, urine volume, and night‑time trips for at least three days.
- Neurological exam: Look for gait instability, cranial nerve deficits, or cognitive slowing.
- Blood tests: Check serum sodium, glucose, and ADH (if available).
- Sleep study (polysomnography) if symptoms of apnea or excessive daytime sleepiness exist.
- Urodynamic testing when neurogenic bladder is suspected to gauge bladder capacity and contractility.
These steps help clinicians decide whether the nocturia stems primarily from the brain injury or from another co‑existing condition.
Practical Management Strategies
Once the cause is clarified, treatment combines three pillars: (1) address the bladder directly, (2) support brain recovery, and (3) optimize sleep.
Bladder‑Specific Interventions
- Timed voiding: Schedule bathroom trips every 2‑3hours during the day to increase daytime output and reduce nighttime urgency.
- Fluid timing: Limit caffeine and alcohol after 6p.m., and aim to finish most fluids two hours before bedtime.
- Anticholinergic meds (e.g., oxybutynin) can calm an overactive bladder, but monitor for cognitive side effects, especially in TBI patients.
- Desmopressin: Synthetic ADH analogue, useful when low ADH is proven; start with low dose and watch sodium levels.
Neuro‑Rehabilitation and Cognitive Support
Physical therapy, occupational therapy, and cognitive rehab improve overall brain function, which in turn can normalize the bladder‑control circuitry.
- Balance exercises reduce fall risk when nighttime bathroom trips are inevitable.
- Memory aids (phone alarms, bathroom lights with motion sensors) minimize the need to stay awake looking for the bathroom.
Sleep‑Optimizing Measures
- CPAP therapy for diagnosed sleep apnea restores proper night‑time oxygenation and reduces nocturnal awakenings.
- Establish a consistent sleep‑wake schedule; avoid screens 30minutes before bed.
- Consider low‑dose melatonin if circadian rhythm is disrupted post‑injury.
When to Seek Professional Help
If you notice any of the following, schedule a follow‑up promptly:
- More than two nightly bathroom trips for three consecutive weeks.
- New or worsening headaches, confusion, or balance problems.
- Sudden weight loss, fever, or blood in the urine (signs of infection).
- Persistent low sodium levels while on desmopressin.
Early intervention can prevent chronic sleep loss, which is linked to mood disorders, cardiovascular disease, and slower brain recovery.
Bottom Line
Head injuries disrupt the very brain networks that tell your kidneys when to hold water and your bladder when to empty. Hormonal shifts, neurogenic bladder, and sleep‑related awakenings all play a part. By tracking symptoms, getting the right tests, and applying a blend of bladder‑focused meds, sleep therapy, and neuro‑rehab, most people can reclaim a full night’s sleep.
Frequently Asked Questions
Can a mild concussion cause nocturia?
Yes. Even a mild concussion can blunt ADH release or cause subtle neurogenic bladder changes, leading to one or two nighttime trips. Monitoring fluid intake and keeping a bladder diary helps determine if the problem is injury‑related.
Is desmopressin safe for people with brain injuries?
Desmopressin can be effective, but it must be prescribed cautiously. Low doses are started, and blood sodium is checked weekly for the first month to avoid hyponatremia, which could worsen cerebral edema.
How does sleep apnea interact with head‑injury‑induced nocturia?
Apnea triggers frequent arousals, each of which can reset the bladder’s urge threshold. Treating apnea with CPAP often reduces nightly trips dramatically, even when the primary cause is a brain injury.
Should I stop drinking water before bed?
Don’t stop altogether-stay hydrated-but aim to finish most fluids two hours before sleep. Small sips are okay if you’re thirsty, and avoid caffeine or alcohol after dinner.
Can medications for other conditions worsen nocturia after a head injury?
Yes. Diuretics, certain antidepressants, and anticholinergics can increase urine output or affect bladder signaling. Review all meds with your clinician; often a dosage tweak or alternative can help.


Debbie Frapp
October 8, 2025 AT 17:39I've been looking into the relationship between traumatic brain injuries and nocturia, and it's fascinating how the neurogenic mechanisms interact with the bladder control pathways. First, the disruption of the pontine micturition center can alter the timing of detrusor muscle activation. Second, impaired autonomic regulation often leads to increased nighttime urine production. Third, sleep fragmentation due to pain or medication can exacerbate the urge to void. Fourth, hormonal imbalances, especially antidiuretic hormone fluctuations, play a role. Fifth, inflammation in the central nervous system can affect the sacral spinal cord segments. Sixth, some patients develop secondary sleep apnea after a head injury, which further increases nocturnal diuresis. Seventh, cognitive deficits may reduce the ability to recognize or suppress the urge to urinate. Eighth, neuroplastic changes might rewire bladder reflexes over time. Ninth, comorbidities such as hypertension can raise renal perfusion pressure at night. Tenth, many clinicians overlook the contribution of fluid management in the acute phase. Eleventh, bladder training protocols need to be adjusted for neurogenic patients. Twelfth, a multidisciplinary approach involving neurologists, urologists, and sleep specialists yields better outcomes. Thirteenth, patient education about timing of fluid intake is crucial. Fourteenth, regular monitoring with bladder diaries helps track progress. Fifteenth, future research should explore targeted neuromodulation to restore normal nocturnal voiding patterns.
Michelle Abbott
October 17, 2025 AT 13:25The pathophysiology is essentially a cascade of neurohormonal dysregulation, leading to nocturnal polyuria via upregulated natriuretic peptide signaling and compromised antidiuretic hormone secretion.
Heather Jackson
October 26, 2025 AT 08:11Wow, thaT’s like a horror movie for your bladder! Imagine waking up every few hours, feeling like a siren at 3 AM, and the doc says, "It’s your brain, girl!" Yup, total drama.
Akshay Pure
November 4, 2025 AT 03:57One must appreciate the elegant elegance of neuro‑urological interplay; the cerebral cortex’s diminished inhibitory tone renders the peripheral urinary apparatus susceptible to dyskinesia, a truly refined observation.
Steven Macy
November 12, 2025 AT 23:43From a philosophical standpoint, the disruption of self‑regulation after a head injury invites us to reconsider how bodily autonomy is mediated by the brain. It’s not merely a symptom; it reflects a deeper disconnection between intention and physiological execution.
Matt Stone
November 21, 2025 AT 19:28Too much fluid before bed = night trips.
Joy Luca
November 30, 2025 AT 15:14Yep, limiting evening drinks can cut those wake‑ups dramatically. Pair that with a short‑term bladder training plan and you’ll see a noticeable drop in nocturia frequency.
Jessica Martins
December 9, 2025 AT 11:00The diagnostic workup should include a post‑void residual measurement and a sleep study, especially if the patient reports snoring or witnessed apneas.
Doug Farley
December 18, 2025 AT 06:46Oh sure, because we all have endless time to schedule polysomnography after a concussion. 🙄
Jeremy Olson
December 27, 2025 AT 02:32In clinical practice, we often start with a thorough history and then proceed to urodynamic testing if nocturia persists beyond the acute recovery phase.
Ada Lusardi
January 4, 2026 AT 22:18💡 Pro tip: Keep a water bottle by the bed, but only sip if you’re really thirsty. It helps avoid the full‑bladder panic at 2 a.m. 😊
Pam Mickelson
January 13, 2026 AT 18:04Great info! Stay positive and remember that small lifestyle tweaks can make a big difference.
Joe V
January 22, 2026 AT 13:50Ah yes, because everyone loves juggling brain rehabilitation with nightly bathroom sprints. Fun times.
Scott Davis
January 31, 2026 AT 09:35True, it adds an extra layer to recovery.