NSAID Gastrointestinal Bleeding Risk Calculator
Assess Your Risk
This tool helps you understand your risk of gastrointestinal bleeding from NSAID use based on key risk factors.
Your Risk Assessment
Every year, millions of people in the U.S. reach for ibuprofen, naproxen, or aspirin to ease a headache, sore knee, or back pain. These drugs - known as NSAIDs - work fast and they’re easy to get. But for many, especially older adults or those with chronic pain, these common painkillers carry a hidden danger: gastrointestinal bleeding. It doesn’t always come with warning signs. Sometimes, it sneaks up as fatigue, dizziness, or iron deficiency anemia. By the time it’s caught, it’s already life-threatening.
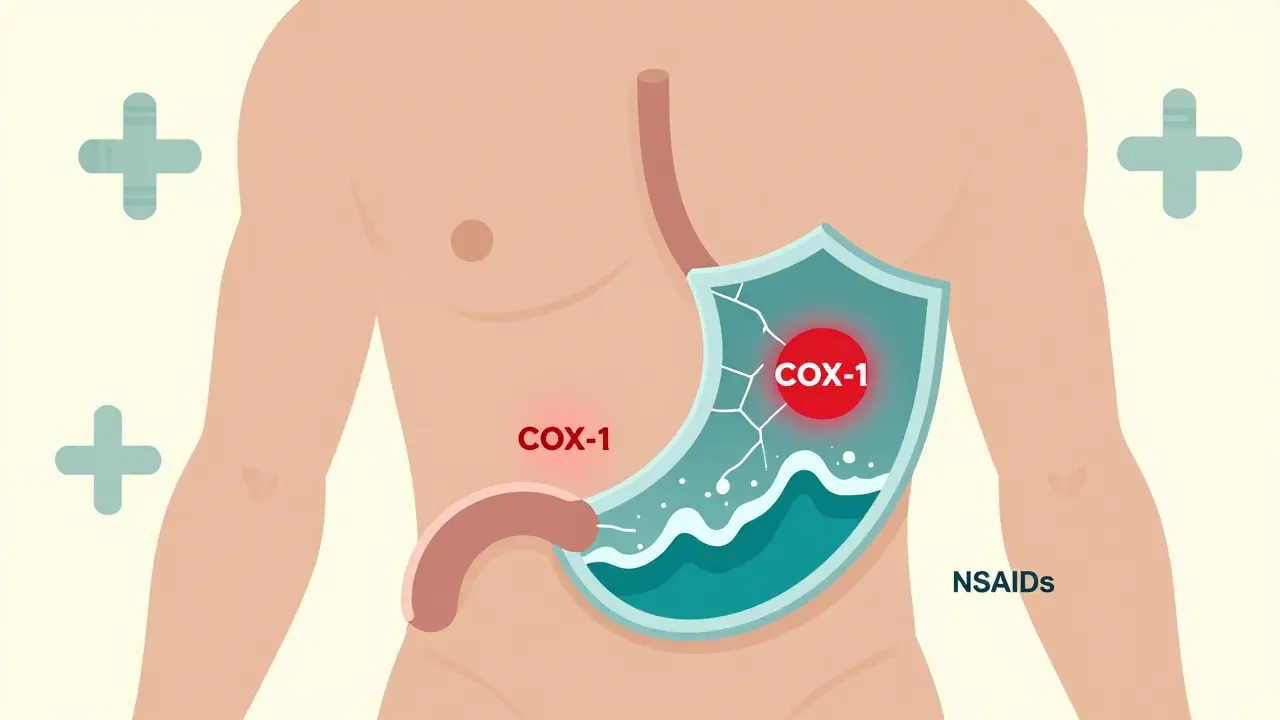
How NSAIDs Damage the Gut
NSAIDs don’t just block pain signals. They shut down two key enzymes: COX-1 and COX-2. COX-2 is linked to inflammation and pain - that’s the target. But COX-1? That’s the enzyme that keeps the stomach lining protected. It helps produce mucus and bicarbonate, the body’s natural shield against stomach acid. When NSAIDs block COX-1, that shield weakens. Acid eats away at the lining. What starts as irritation can turn into an ulcer - or worse, a bleed.It’s not just the stomach. NSAIDs can hurt the entire digestive tract - from the esophagus down to the small intestine. Studies show that up to 86% of people with lower GI bleeding had taken NSAIDs, even if they didn’t have a visible ulcer. That means you don’t need a classic peptic ulcer to bleed. Tiny erosions, invisible on a scope, can still leak blood slowly over weeks. That’s how people end up with low iron and no idea why.
Who’s at Highest Risk?
Not everyone who takes NSAIDs bleeds. But some people are far more vulnerable. The risk isn’t random - it’s predictable. Experts have identified clear warning signs:- Age 70 or older - risk doubles every decade after 60
- History of peptic ulcer or prior GI bleed - this is the biggest red flag
- Taking blood thinners like warfarin or apixaban - doubles the bleeding risk
- Using corticosteroids (like prednisone) at the same time - adds another layer of danger
- Taking more than one NSAID at once - including OTC and prescription
- Daily doses over 1,200 mg of ibuprofen or equivalent
A 2021 American College of Gastroenterology tool gives each of these factors points. Two or more points? You’re in the high-risk zone. That’s not a suggestion - it’s a medical emergency waiting to happen.
NSAID Types: Not All Are Equal
The idea that all NSAIDs are the same is dangerous. There’s a big difference between ibuprofen and celecoxib.Traditional NSAIDs like naproxen, diclofenac, and ibuprofen block both COX-1 and COX-2. That’s why they’re so hard on the gut. In contrast, COX-2 inhibitors like celecoxib (Celebrex) and etoricoxib were designed to spare COX-1. A 2000 Lancet study found celecoxib cut complicated ulcers by half compared to ibuprofen. But here’s the catch: COX-2 inhibitors raise heart attack risk. The rofecoxib (Vioxx) scandal in 2004 wasn’t an outlier - it changed how we think about these drugs.
Today, COX-2 inhibitors are still used, but only for patients who absolutely need them and have no heart disease. For someone with arthritis and a history of ulcers? The safest path isn’t just picking a different NSAID - it’s adding protection.

Protection That Actually Works
If you’re at risk and need NSAIDs, you don’t have to suffer in silence. There are proven ways to reduce harm.Proton pump inhibitors (PPIs) like omeprazole, esomeprazole, or pantoprazole are the gold standard. A 2017 Cochrane review of over 13,000 patients found PPIs cut NSAID-related ulcers by 75%. That’s not a small benefit - it’s life-saving. Starting a PPI before the NSAID gives the best protection. Waiting until symptoms appear? Too late.
Misoprostol (Cytotec) also reduces ulcers by 50-75%, but it’s tough to tolerate. Diarrhea hits nearly 1 in 5 people. Abdominal cramps are common. Most patients quit it within weeks.
Then there’s Vimovo - a single pill combining naproxen and esomeprazole. Approved in 2023, it’s designed for high-risk patients. In a 2022 trial, it slashed ulcer complications from 25.6% to just 7.3% compared to naproxen alone. It’s not cheap, but for someone who’s bled before, it’s worth the cost.
The Silent Bleed: When You Don’t Know It’s Happening
The scariest part? Most people don’t realize they’re bleeding.One patient on Reddit, u/ElderCareHelper, shared how their 78-year-old mother ended up in the ER after fainting at home. Her hemoglobin had dropped to 6.8 g/dL - critically low. She’d been taking ibuprofen daily for arthritis for three years. No stomach pain. No black stools. Just fatigue and shortness of breath. She needed three units of blood. The cause? A slow bleed from a small bowel ulcer caused by NSAIDs.
A 2022 Arthritis Foundation survey found 42% of NSAID users stopped taking them because of gut symptoms. But 63% of patients on HealthUnlocked reported GI issues and never told their doctor. Why? They think it’s normal. Or they’re afraid to stop pain relief. Or they don’t know NSAIDs can do this.
That’s the gap. We treat the pain, not the side effect. We need to change that.
What Should You Do?
If you’re taking NSAIDs regularly - even just a couple of times a week - here’s what to ask yourself:- Am I over 65?
- Have I ever had an ulcer or GI bleed?
- Am I on blood thinners or steroids?
- Do I take more than one NSAID at a time?
If you answered yes to two or more, talk to your doctor. Don’t wait for symptoms. Get a PPI prescription. Consider switching to a COX-2 inhibitor with PPI if you’re at high risk. Ask about Vimovo if you’re on naproxen.
If you’re under 65, healthy, and only use NSAIDs occasionally - you’re likely fine. But don’t assume. If you notice dark stools, unexplained fatigue, or dizziness when standing, get checked. A simple blood test can catch anemia before it’s an emergency.
What’s Next?
Science is moving forward. New drugs called CINODs - like naproxcinod - are in late-stage trials. They release nitric oxide along with NSAID action, which helps protect the gut lining. Early results show 50% fewer ulcers than traditional NSAIDs. But they’re still years away from market.For now, the answer isn’t to avoid NSAIDs entirely. It’s to use them smarter. The American College of Rheumatology now recommends the lowest dose for the shortest time possible - even for chronic conditions. For many, physical therapy, weight management, or acetaminophen might be safer first steps.
NSAIDs are powerful tools. But they’re not harmless. The same pills that help you walk again can quietly damage your gut. Awareness isn’t enough. Action is.
Can over-the-counter NSAIDs cause gastrointestinal bleeding?
Yes. Over-the-counter NSAIDs like ibuprofen and naproxen are just as likely to cause bleeding as prescription versions. In fact, 26% of users take them at doses higher than recommended, and many don’t tell their doctors. Bleeding doesn’t care if the drug was bought at a pharmacy or prescribed by a physician.
Is it safe to take aspirin with other NSAIDs?
No. Aspirin is itself an NSAID and blocks COX-1. Taking it with another NSAID - even low-dose daily aspirin for heart protection - doubles the risk of bleeding. If you need both, talk to your doctor about adding a PPI. Never combine them without medical advice.
Do COX-2 inhibitors like Celebrex cause less bleeding than ibuprofen?
Yes, they do. Studies show COX-2 inhibitors reduce the risk of serious ulcers and bleeding by about 50% compared to traditional NSAIDs like ibuprofen. But they come with a trade-off: higher heart attack risk. They’re only recommended for people with high GI risk and low heart disease risk.
How long does it take for NSAIDs to cause a bleed?
There’s no set timeline. Some people bleed after just a few days, especially if they’re high-risk. Others take months or years. The damage builds slowly. That’s why regular users - even without symptoms - should be monitored. Occult bleeding can lead to anemia before any pain or dark stools appear.
Can I stop NSAIDs cold turkey if I’m worried about bleeding?
If you’re taking NSAIDs for chronic pain like arthritis, stopping suddenly can cause a flare-up. Don’t quit without talking to your doctor. Instead, ask about switching to a safer option - like a COX-2 inhibitor with PPI, or non-NSAID alternatives such as physical therapy, topical pain relievers, or acetaminophen.
Are there natural alternatives to NSAIDs for pain?
Yes. For joint pain, options include physical therapy, weight loss, heat/cold therapy, and topical capsaicin or menthol creams. Turmeric and omega-3 supplements show mild anti-inflammatory effects, but they’re not as strong as NSAIDs. For acute pain, acetaminophen (Tylenol) is a safer choice for the gut - though it doesn’t reduce inflammation.
What are the signs of a slow, hidden NSAID bleed?
Fatigue, weakness, shortness of breath, pale skin, and dizziness when standing are common. You might feel like you’re always tired, even after sleeping. A simple blood test showing low hemoglobin or iron levels can reveal an occult bleed - even if you feel fine otherwise.
Should I get an endoscopy if I’ve been on NSAIDs for years?
Not routinely - unless you have symptoms like black stools, vomiting blood, or unexplained anemia. But if you’re high-risk (age 70+, prior ulcer, on blood thinners), your doctor may recommend a baseline scope before starting long-term NSAIDs. Prevention is better than waiting for a crisis.

Mark Able
December 19, 2025 AT 03:15I took ibuprofen for my back for years and never thought twice until I passed out at the grocery store. Hemoglobin was 5.9. Turns out I had a slow bleed from a tiny ulcer. No pain. No warning. Just constant tiredness. Doc said if I’d waited another week I might not have made it. NSAIDs are not harmless. Period.
Chris Clark
December 19, 2025 AT 07:34Man I just found out my grandma was on naproxen for 8 years and never told anyone she was always dizzy and pale. She thought it was just getting old. She ended up in the ER with a transfusion. Now she’s on Vimovo and feels like a new person. Why isn’t this common knowledge? Like, why do we treat pain like it’s the only thing that matters? The gut doesn’t scream, it just fades away.
Dorine Anthony
December 21, 2025 AT 06:03My dad’s on daily aspirin for his heart and takes ibuprofen for his knees. He says it’s fine because he’s only taking a couple. But I looked it up and now I’m terrified. He’s 72, on both, and never told his doctor. I’m gonna make him go in next week. This stuff is silent.
William Storrs
December 22, 2025 AT 16:47Listen. If you’re over 65 and still popping NSAIDs like candy, you’re playing Russian roulette with your insides. PPIs aren’t optional. They’re your body’s seatbelt. Don’t wait until you’re in the hospital with a bag of blood hanging from your arm. Talk to your doc. Get a script. Start today. Your future self will thank you. Seriously. Just do it.
James Stearns
December 24, 2025 AT 06:04It is an incontrovertible fact that the indiscriminate use of nonsteroidal anti-inflammatory agents constitutes a grossly negligent public health oversight. The pharmacological mechanism of cyclooxygenase-1 inhibition is not merely a side effect-it is a systemic erosion of mucosal integrity. The absence of symptomatic presentation does not equate to the absence of pathophysiological damage. One must exercise rigorous clinical prudence when prescribing or self-administering such agents. This is not a lifestyle choice-it is a medical imperative.
Nina Stacey
December 26, 2025 AT 01:37So basically if you’re old and in pain you’re just supposed to suffer? I mean I get it PPIs work but they’re like a bandaid on a bullet wound. And don’t even get me started on Vimovo - $300 a month? That’s a joke. My cousin’s on it and she’s broke now. We need cheaper options. Like real ones. Not just fancy pills with fancy names that only rich people can afford. This whole thing is messed up.
Dominic Suyo
December 26, 2025 AT 13:01Let’s be real - NSAIDs are the opioid of the 2020s. Everyone’s on them, nobody talks about the damage, and the pharma companies are laughing all the way to the bank. COX-2 inhibitors? More like COX-2 *bombs*. And PPIs? You think you’re protected? Try dealing with 3 years of bloating, vitamin B12 deficiency, and C. diff because you were ‘just taking omeprazole for safety’. We’re not fixing the problem. We’re just layering on more side effects. This system is broken.
Kevin Motta Top
December 28, 2025 AT 02:43Acetaminophen for mild pain. Physical therapy for joints. Topical creams. These are the real first steps. NSAIDs should be the last resort - not the first.