When you’re seriously ill, your body doesn’t just feel bad-it changes how your hormones work. One of the most misunderstood changes happens in your thyroid lab results. You might see low T3, low T4, or even a weirdly high reverse T3, and your doctor might think you have hypothyroidism. But here’s the catch: your thyroid gland is perfectly fine. This isn’t a thyroid problem. It’s sick euthyroid syndrome.
What Actually Happens When You’re Sick?
Sick euthyroid syndrome, also called nonthyroidal illness syndrome (NTIS), isn’t a disease. It’s your body’s way of slowing down. When you’re fighting sepsis, recovering from major surgery, or dealing with a heart attack, your body doesn’t have the energy to keep your metabolism running full speed. So it turns down the thyroid signal-not because the gland is broken, but because it’s trying to save you. This isn’t theoretical. About 70-75% of people in intensive care units show these abnormal thyroid labs. The more sick you are, the more likely it is to show up. In sepsis? Up to 85% of patients. Severe burns? Nearly 80%. Even in chronic conditions like liver cirrhosis or anorexia nervosa, it’s common. The real clue? Your TSH-the hormone your brain sends to tell your thyroid to work-stays normal. Or maybe it’s slightly low or slightly high, but not in the way you’d expect if your thyroid were failing. That’s the first red flag: if your TSH is normal while T3 and T4 are low, it’s almost certainly not primary hypothyroidism.What the Labs Look Like
Here’s what you’ll typically see on a blood test when sick euthyroid syndrome is present:- Low T3-This is the most consistent finding. In 95% of cases, your active thyroid hormone drops. Your body stops converting T4 into T3, which is the form your cells actually use.
- Low T4-Appears in about half the cases, especially if the illness lasts longer than a few days.
- High reverse T3 (rT3)-Your body makes more of this inactive form of T3, which blocks the active hormone from working. It’s like putting a lock on your thyroid signal.
- Normal or mildly abnormal TSH-Usually stays between 0.4 and 4.0 mIU/L. Sometimes it dips below 0.4 in acute illness, or creeps up to 5-10 during recovery. But it doesn’t go sky-high like in Hashimoto’s.
Why It Mimics Hypothyroidism
The symptoms can be almost identical: fatigue, feeling cold, constipation, muscle weakness. In severe cases, people get low body temperature, slow breathing, low blood pressure, or even confusion. It’s easy to see why someone might think, “This is hypothyroidism.” But here’s what’s missing: no goiter. No dry skin or hair loss. No elevated thyroid antibodies. No history of autoimmune disease. No weight gain that doesn’t match your calorie intake. These are the signs of true thyroid failure. In sick euthyroid syndrome, your body is conserving energy-not failing. In fact, research shows that lowering your metabolic rate by 15-20% during severe illness might actually help you survive. Your body redirects energy to healing, immune response, and vital organ function instead of digestion, movement, or heat production.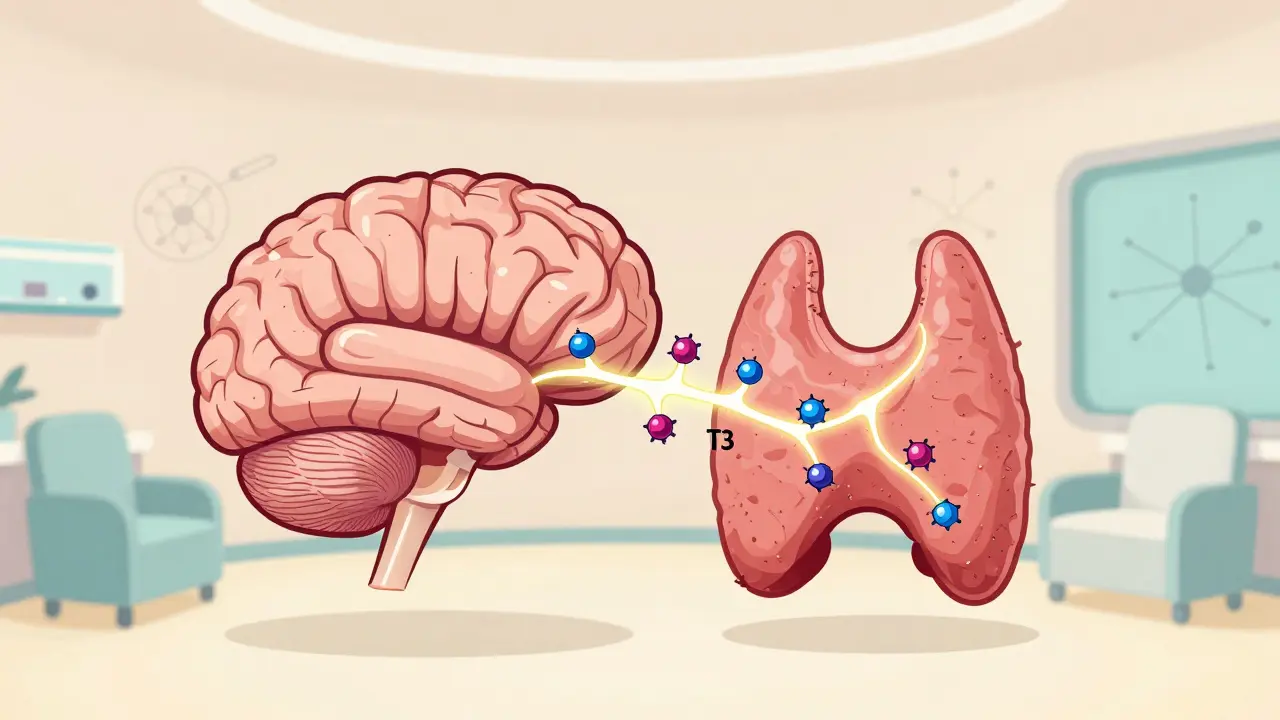
Why Treating It Makes Things Worse
This is the most important part: you should not take thyroid medication for sick euthyroid syndrome. In a 2022 clinical trial with 450 critically ill patients, those given levothyroxine had the same 30-day death rate as those who got a placebo. Their time in the ICU? Identical. Their recovery speed? No difference. And here’s the scary part: giving thyroid hormone to someone with ESS can backfire. A 2021 study of 3,200 ICU patients found that 12% were incorrectly diagnosed with hypothyroidism and given thyroid pills. Those patients had worse outcomes-higher risk of heart rhythm problems, longer hospital stays, and higher death rates. The American Thyroid Association and the Endocrine Society both say the same thing: don’t treat it. Treat the illness. If you’re in the hospital with pneumonia, treat the pneumonia. If you’re recovering from surgery, focus on healing. The thyroid labs will fix themselves once you’re better.When to Be Concerned
There are times when abnormal thyroid labs mean something else. If your TSH is low AND your T3 and T4 are low, that’s not sick euthyroid syndrome-that’s central hypothyroidism, which is rare and needs treatment. If your TSH is very high (above 10) with low T4, that’s likely Hashimoto’s. Also, if your thyroid labs stay abnormal for more than 4-6 weeks after you’ve recovered from your illness, you should get retested. Persistent changes could mean you actually have an underlying thyroid disorder that was masked by the acute illness.


Jon Paramore
December 20, 2025 AT 18:03Let’s cut through the noise: sick euthyroid syndrome isn’t a glitch-it’s a feature. Your body isn’t broken, it’s optimizing. When cytokines spike, deiodinase enzymes get shut down on purpose. T3 plummets because your cells don’t need energy for gym sessions or late-night scrolling. They need it for macrophages and fever responses. TSH stays normal because the hypothalamus isn’t confused-it’s strategic. Giving T4? That’s like adding fuel to a fire you’re trying to smother. The data’s clear: no benefit, more risk. Stop treating labs. Treat patients.
Jason Silva
December 22, 2025 AT 08:06Bro this is wild 😳 I had a friend in ICU last year and they gave him levothyroxine because his T3 was low. He ended up in AFib for 3 days. They didn’t even check if he was actually sick or just ‘thyroid broken’. The system is rigged. Big Pharma loves labeling everything as ‘hypothyroid’ so they can sell you pills forever. 🤡
Stacey Smith
December 24, 2025 AT 05:18My uncle got pumped full of thyroid meds during his sepsis recovery. Turned out he didn’t need it. Just got worse. Now he’s on a permanent dose because the doc didn’t know the difference. This is why people get addicted to meds they don’t need.
Adrian Thompson
December 25, 2025 AT 03:02So let me get this straight-your body’s natural survival mechanism is being called a ‘syndrome’ so doctors can profit off treating it? Classic. They don’t want you to heal naturally. They want you on lifelong meds. This is just another way the medical-industrial complex keeps you dependent. Next they’ll say your fever is ‘unhealthy’ and prescribe acetaminophen to stop your immune system. Wake up.
Cameron Hoover
December 25, 2025 AT 06:45It’s beautiful, really. Evolution didn’t design our bodies to be optimized for productivity-it designed them to survive. When you’re down, your body doesn’t care about your LinkedIn goals or your six-pack. It’s shutting down the non-essentials so you can live to fight another day. That’s not disease. That’s wisdom. We’ve forgotten how to listen to our bodies because we’re too busy chasing metrics.
Peggy Adams
December 26, 2025 AT 05:07So… you’re saying if I’m sick and my T3 is low, I shouldn’t take thyroid pills? That’s it? That’s the whole post? I thought this was gonna be a deep dive. Boring.
Hannah Taylor
December 27, 2025 AT 21:51wait so reverse t3 is like… a fake hormone? so they just make it up? why do labs even test for it then? i think this is all a scam. i read on a forum that the FDA hides the truth about t3 because big pharma owns the labs. also my cousin’s dog had low t3 and got better after eating kale. so…
Ben Warren
December 28, 2025 AT 04:54It is imperative to underscore, with the utmost scholarly rigor, that the pathophysiological underpinnings of nonthyroidal illness syndrome (NTIS) are not merely a matter of metabolic downregulation, but rather a complex, multi-tiered neuroendocrine adaptation mediated by the hypothalamic-pituitary-thyroid axis in response to systemic inflammatory burden. The suppression of 5'-deiodinase type I activity, concomitant with increased expression of type III deiodinase and diminished thyroid hormone-binding globulin affinity, constitutes a highly conserved evolutionary survival mechanism. To administer exogenous thyroid hormone in this context is not merely ineffective-it is a violation of the principle of primum non nocere. The literature, including the 2022 Endocrine Society guidelines and the EUTHYROID-ICU prospective cohort, unequivocally supports non-intervention. Any deviation from this standard constitutes medical malpractice in the context of critical illness.
Teya Derksen Friesen
December 29, 2025 AT 01:45This is one of those rare moments where medicine actually makes sense. Not everything needs a pill. Not every abnormal lab means disease. Sometimes, the body knows what it’s doing better than the test strip. I wish more doctors would pause before prescribing.
Sandy Crux
December 29, 2025 AT 23:29...and yet, despite the overwhelming evidence, the American Thyroid Association still allows thyroid testing in ICU settings-because, of course, they’re influenced by pharmaceutical lobbying. The fact that this isn’t universally enforced as a guideline speaks volumes about the rot within institutional medicine. You can’t fix a system that profits from misdiagnosis. The ‘normal’ range is arbitrary. The ‘reference’ population is biased. And you-yes, you-are being manipulated.
mukesh matav
December 30, 2025 AT 06:38My father was in the hospital for pneumonia last winter. They tested his thyroid. T3 was low. We asked if it was sick euthyroid. The nurse looked confused. He was given no meds. He recovered in 10 days. I’m glad we didn’t push for more tests. Sometimes less is more.
Theo Newbold
December 31, 2025 AT 21:14Let’s not romanticize this. This isn’t ‘wisdom.’ It’s a stress response. And stress responses are dangerous when prolonged. The fact that T3 stays low for weeks in some patients after recovery? That’s not adaptive-it’s pathological. You’re ignoring the fact that prolonged low T3 correlates with muscle wasting, cognitive decline, and increased mortality in non-critical patients. This isn’t a ‘don’t treat’ situation-it’s a ‘monitor and intervene if persistent’ situation. Oversimplification kills.
Sarah Williams
January 2, 2026 AT 05:18Thank you for writing this. I’ve seen too many people panic over thyroid results after being sick. You’re right-it’s not a problem. It’s a pause. Let your body breathe. Healing isn’t linear. And sometimes, the best thing you can do is nothing at all.
Swapneel Mehta
January 4, 2026 AT 01:34Interesting how the body knows when to slow down. We spend so much time pushing ourselves-work, hustle, grind-but when we’re truly sick, nature just says: rest. No pills. No fixes. Just time. Maybe we should listen more often.