Heartburn Risk Calculator
Your Risk Factors
Heartburn Risk Assessment
Heartburn isn’t just a nuisance after a big meal-it’s a signal your body is struggling with something deeper. If you’re eating spicy foods and taking medications like aspirin, ibuprofen, or even blood pressure pills, you might be stacking two triggers that make heartburn worse. And while antacids give quick relief, they don’t fix the root problem. The real solution? Understanding how these triggers interact and adjusting both your diet and medication habits to protect your digestive system.
Why Spicy Food Makes Heartburn Worse
It’s not just about the heat. The compound that makes chili peppers spicy-capsaicin-directly affects the muscle that keeps stomach acid where it belongs: the lower esophageal sphincter (LES). When this muscle relaxes too much, acid flows back into your esophagus, causing that burning sensation. Studies show capsaicin can drop LES pressure by 30-40% in sensitive people within 30 minutes of eating. That’s why even a small bite of hot salsa can trigger symptoms for some, while others eat buffalo wings without issue.
The NIH says there’s not enough evidence to ban spicy food for everyone with GERD. But clinical experience tells a different story. Dr. Kyle Staller from Massachusetts General Hospital found that 65-75% of GERD patients report worse symptoms after eating spicy meals. It’s not a universal rule, but it’s common enough to warrant testing. If you notice heartburn after chili, curry, or hot sauce, it’s worth cutting it out for 3-7 days to see if things improve.
Medications That Make Heartburn Worse
Many common drugs aren’t designed to hurt your stomach-but they do. Aspirin and ibuprofen (NSAIDs) can cause tiny erosions in the esophagus and increase acid production. Regular use raises GERD risk by 40-60%. Beta blockers, often prescribed for high blood pressure, relax the LES and increase heartburn risk by 22%, according to the Framingham Heart Study. Even medications for asthma (theophylline) and chest pain (nitrates) can loosen the LES by up to 45%.
Anticholinergics, used for motion sickness or overactive bladder, are another hidden culprit. A University of Michigan study found they reduce LES pressure in 68% of users. And if you’re taking bisphosphonates for osteoporosis, you’re at risk for esophagitis-especially if you take them lying down or with too little water.
It’s not just about what you take-it’s when. Taking these meds right before bed or on an empty stomach increases the chance of acid damage. Always take NSAIDs with food and water, and avoid lying down for at least 30 minutes after swallowing them.
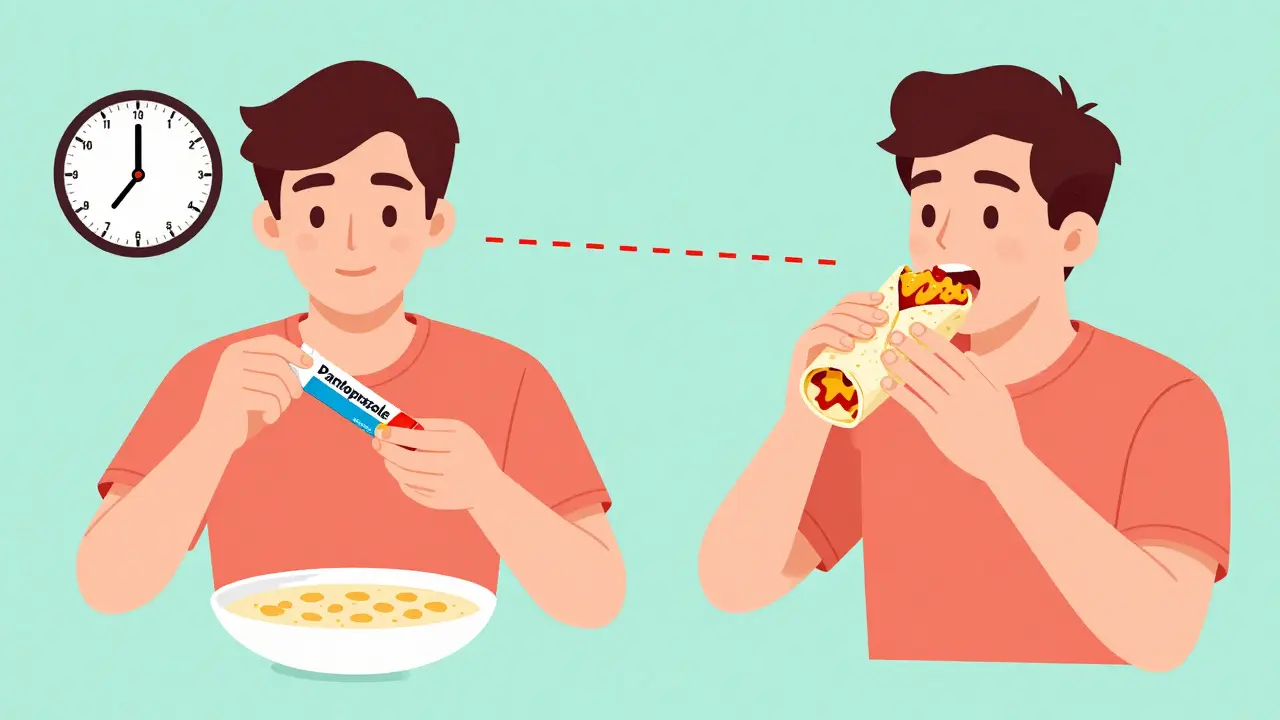
How Medications Like Pantoprazole Lose Their Edge
Pantoprazole, a proton pump inhibitor (PPI), is one of the most prescribed drugs for heartburn. But it doesn’t work the same way if you eat spicy, fatty, or acidic foods soon after taking it. Research shows its absorption drops by 18-23% when taken within two hours of trigger foods. That means you might be taking your pill correctly-but eating a spicy burrito an hour later, and your medication isn’t doing its job.
For maximum effect, take pantoprazole 30-60 minutes before your first meal of the day. Don’t wait until after breakfast. And avoid pairing it with coffee, chocolate, alcohol, or mint-these also interfere with absorption. If you’re still having symptoms despite taking your PPI, your diet might be sabotaging it.
Also, don’t rely on PPIs long-term without checking in with your doctor. Chronic use has been linked to increased risks of kidney disease, bone fractures, and nutrient deficiencies. The FDA has flagged potential heart attack risks, too. That’s why more doctors are now pushing for lifestyle changes before increasing medication doses.
Antacids: Quick Fix, Long-Term Risk
When heartburn hits, Tums or Rolaids feel like magic. They neutralize acid in 2-5 minutes. But their effect lasts only 30-60 minutes. That’s why so many people end up taking them repeatedly after spicy meals. The problem? Overusing antacids can cause electrolyte imbalances, especially if you’re using aluminum- or magnesium-based ones daily.
Worse, antacids interfere with other meds. Aluminum in Tums can cut tetracycline antibiotic absorption by half. Fluoroquinolones like Cipro lose up to 90% of their strength if taken with antacids. The Cleveland Clinic recommends spacing antacids at least four hours apart from other medications. If you’re on multiple prescriptions, this timing matters.
And here’s a hidden danger: antacids mask symptoms. If you’re popping them after every spicy meal, you might be ignoring a hiatal hernia, Barrett’s esophagus, or even early signs of esophageal damage. Heartburn that keeps coming back isn’t just annoying-it’s a warning.
What Actually Works: A Practical Plan
There’s no one-size-fits-all fix. But a proven approach combines timing, testing, and smart habits.
- Track your triggers. Keep a food and symptom diary for two weeks. Note everything you eat, when you took meds, and if heartburn followed. Look for patterns-not just spicy food, but also timing, portion size, and posture after eating.
- Eliminate and reintroduce. Cut out spicy foods, caffeine, alcohol, and chocolate for 7 days. Then add one back every 3 days. If symptoms return, you’ve found your trigger.
- Time your meds right. Take PPIs 30-60 minutes before breakfast. Take antacids at least 4 hours after other pills. Avoid NSAIDs on an empty stomach.
- Change your habits. Don’t lie down for 3 hours after eating. Elevate the head of your bed by 6-8 inches. Eat smaller meals spaced 3 hours apart. This reduces stomach pressure and helps your body empty food properly.
- Try capsaicin desensitization. If you love spicy food, some people can rebuild tolerance. Start with very mild heat (like paprika) and slowly increase over weeks. Johns Hopkins research showed 65% of participants improved their tolerance without flare-ups after 12 weeks.
Patients who follow this personalized plan have a 78% success rate controlling symptoms, according to Dr. Lauren B. Gerson’s 2023 meta-analysis. Those who rely only on meds? Only 42% get lasting relief.

What’s New in GERD Treatment
The field is shifting away from blanket restrictions. The American Gastroenterological Association’s 2023 guidelines now support “precision nutrition”-tailoring advice to your body, not a list of forbidden foods. And new drugs are emerging. Vonoprazan (Voquezna), approved by the FDA in August 2023, works faster and more consistently than traditional PPIs, even in people who don’t respond well to older meds.
At the same time, the market is changing. Prescription PPI sales are growing slowly, while diet and lifestyle programs are booming. Hospitals that hire dietitians to work with GERD patients see 27% lower medication costs and 33% better outcomes. The future of heartburn care isn’t just more pills-it’s smarter eating, better timing, and personal insight.
When to See a Doctor
Heartburn that happens more than twice a week, wakes you up at night, or doesn’t respond to OTC meds needs evaluation. So does trouble swallowing, unexplained weight loss, or vomiting blood. These aren’t normal. They could signal Barrett’s esophagus, a precancerous condition, or a hiatal hernia.
If you’re on long-term PPIs, ask your doctor about getting off them safely. Stopping suddenly can cause rebound acid hypersecretion-where your stomach overproduces acid, making symptoms worse than before. A gradual taper, paired with dietary changes, is safer.
Can spicy food cause permanent damage to the esophagus?
Spicy food itself doesn’t cause permanent damage, but chronic acid reflux from repeated triggers can. Over time, stomach acid eroding the esophagus lining can lead to Barrett’s esophagus, a condition that increases cancer risk. Spicy food is a trigger, not the direct cause-but if it’s making your reflux worse, it’s contributing to the damage.
Is it safe to take antacids every day?
No. Taking antacids more than 2-3 times a week can lead to electrolyte imbalances, kidney problems, or interfere with other medications. They’re meant for short-term relief, not daily management. If you need them often, talk to your doctor about underlying causes and better long-term options.
Does drinking water help reduce heartburn after spicy food?
Water can help wash acid down and dilute it slightly, but it won’t neutralize capsaicin or fix a relaxed LES. Milk or yogurt may offer more relief because they contain fats that bind to capsaicin. Still, the best strategy is prevention-avoiding triggers or spacing them from medications.
Can I still eat spicy food if I’m on pantoprazole?
You might, but it depends. If your PPI isn’t working as well, spicy food could be why. Try taking your pill 30-60 minutes before your meal, then wait at least 2 hours before eating anything spicy. If symptoms still happen, you may need to reduce your spice level or find alternatives like smoked paprika instead of cayenne.
How long does it take to see improvement after changing my diet?
Most people notice improvement within 1-2 weeks of eliminating triggers and adjusting medication timing. Full symptom control often takes 3-4 weeks, especially if you’re also tapering off PPIs. Consistency is key-track your meals and symptoms daily to spot patterns.
Final Thought: Your Body, Your Rules
Heartburn isn’t something you just have to live with. It’s not a punishment for loving spicy food or taking necessary meds. It’s a clue. Your body is telling you that something in your routine isn’t working. The goal isn’t to give up everything you love-it’s to find your personal balance. Test your triggers. Time your meds. Listen to your body. And don’t settle for masking symptoms with pills when real change is possible.


Herman Rousseau
December 22, 2025 AT 17:11Been dealing with this for years. Took me 3 months of tracking to realize my nightly ibuprofen for back pain was wrecking my esophagus. Switched to acetaminophen and cut out spicy dinners after 7pm. No more midnight burning. PPIs are not a license to eat tacos at midnight.