Chlamydia Arthritis Link: What Happens When Infection Hits Your Joints
When dealing with chlamydia arthritis link, the connection between a chlamydia infection and joint inflammation that leads to reactive arthritis. Also known as chlamydia‑associated reactive arthritis, it is a type of reactive arthritis, an autoimmune‑driven joint disease that follows an infection elsewhere in the body, often triggered by a sexually transmitted infection, a disease passed through sexual contact, like chlamydia. Understanding how these pieces fit together helps you spot problems early and get the right care.
Why a Simple Bacterial Infection Can Spark Joint Pain
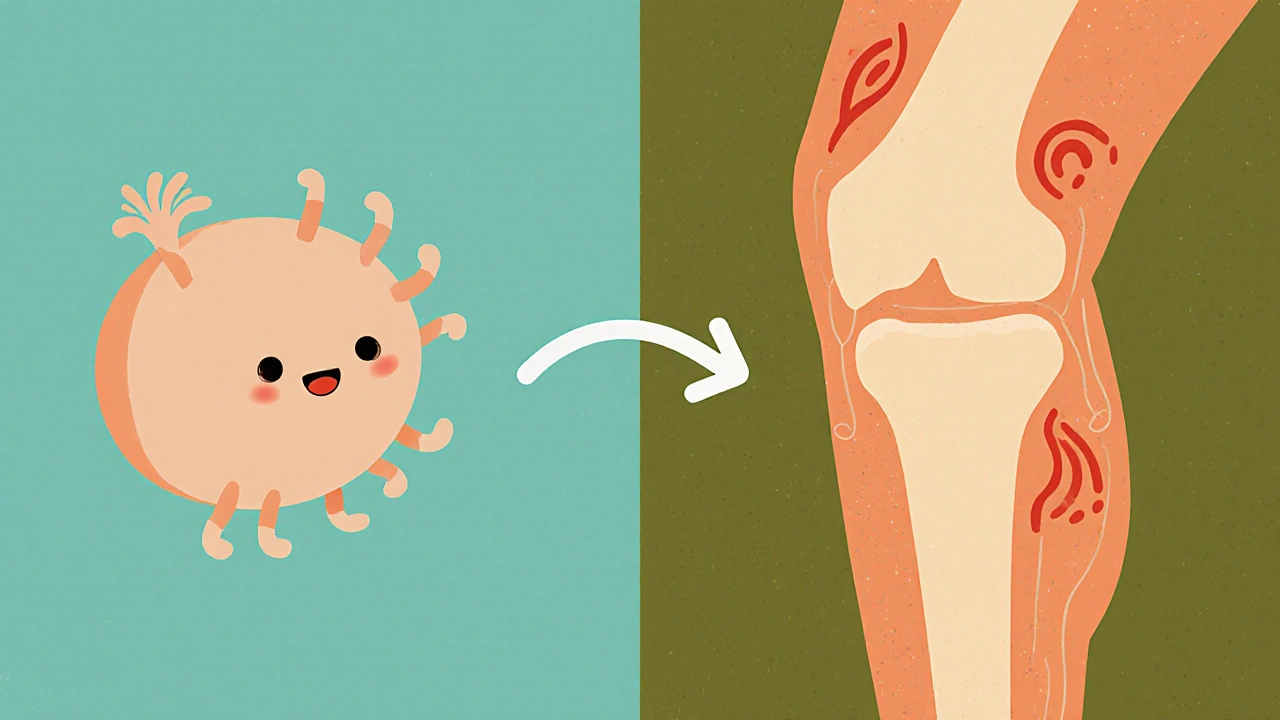
The chlamydia arthritis link hinges on the body’s immune response. Chlamydia trachomatis, the bacteria behind most chlamydia cases, settles in the genital tract but can also travel to distant sites. Once there, the immune system launches a full‑blown attack, mistaking joint tissue for the invader. This misdirected response creates inflammation, swelling, and stiffness in the knees, ankles, or toes. Key attributes of this reaction include a sudden onset, asymmetric joint involvement, and often accompanying skin or eye symptoms. In other words, the infection acts as a trigger, while the actual joint damage comes from the body’s own defense mechanisms.
Symptoms usually appear weeks after the initial infection. You might notice pain that worsens with movement, warmth around the joint, or a lingering ache that doesn’t improve with rest. Because the infection itself can be silent, many people never suspect a link to their joint issues. That’s why recognizing the pattern—recent STI, followed by joint complaints—is crucial for a correct diagnosis.
Diagnosing the chlamydia arthritis link starts with a thorough medical history and a physical exam focused on joint tenderness and range of motion. Laboratory tests play a big role: nucleic acid amplification tests (NAAT) on urine or genital swabs confirm chlamydia, while blood work looks for markers of inflammation like ESR or CRP. Imaging such as X‑ray or MRI can rule out other joint diseases and show characteristic signs of reactive arthritis, like enthesitis (inflammation where tendons attach to bone). Putting these pieces together lets doctors pinpoint the infection‑driven arthritis rather than mistaking it for rheumatoid arthritis or gout.
Treatment tackles two fronts: eradicating the chlamydia and calming joint inflammation. A standard 7‑day course of doxycycline or a single dose of azithromycin clears the bacterial infection in most cases. For the arthritis itself, non‑steroidal anti‑inflammatory drugs (NSAIDs) reduce pain and swelling. If symptoms persist, short courses of oral steroids or disease‑modifying agents may be prescribed. Physical therapy also helps restore mobility and prevent stiffness. Early intervention usually leads to a full recovery, but some people may experience lingering joint issues that need long‑term management.
Prevention is straightforward: practicing safe sex, using condoms, and getting regular STI screenings cut the risk of chlamydia and, by extension, the arthritis it can provoke. If you catch a chlamydia infection early, prompt antibiotic treatment often stops the cascade before the immune system turns on the joints. Education and awareness are your best tools for keeping both your reproductive and musculoskeletal health in check.
Below, you’ll find a curated collection of articles that dive deeper into related topics—pain relief options, infection‑related skin conditions, and more. Whether you’re looking for treatment comparisons, lifestyle tips, or the science behind how infections affect the body, these posts are organized to give you quick, actionable information.
Chlamydia and Reactive Arthritis: Understanding the Link
Explore how chlamydia infection can trigger reactive arthritis, covering symptoms, diagnosis, treatment, and prevention.
