Why anabolic agents are changing osteoporosis care
For years, osteoporosis treatment was all about slowing bone loss. Drugs like bisphosphonates and denosumab kept bones from breaking down too fast, but they didn’t rebuild what was already gone. That changed when the FDA approved teriparatide in 2002-the first true bone-building drug. Then came abaloparatide in 2017, offering a more targeted approach. These aren’t just new pills. They’re daily injections that actually stimulate your body to make new bone. For people with severe osteoporosis, especially those who’ve already broken a bone, this isn’t just an option-it’s a turning point.
How teriparatide and abaloparatide work differently
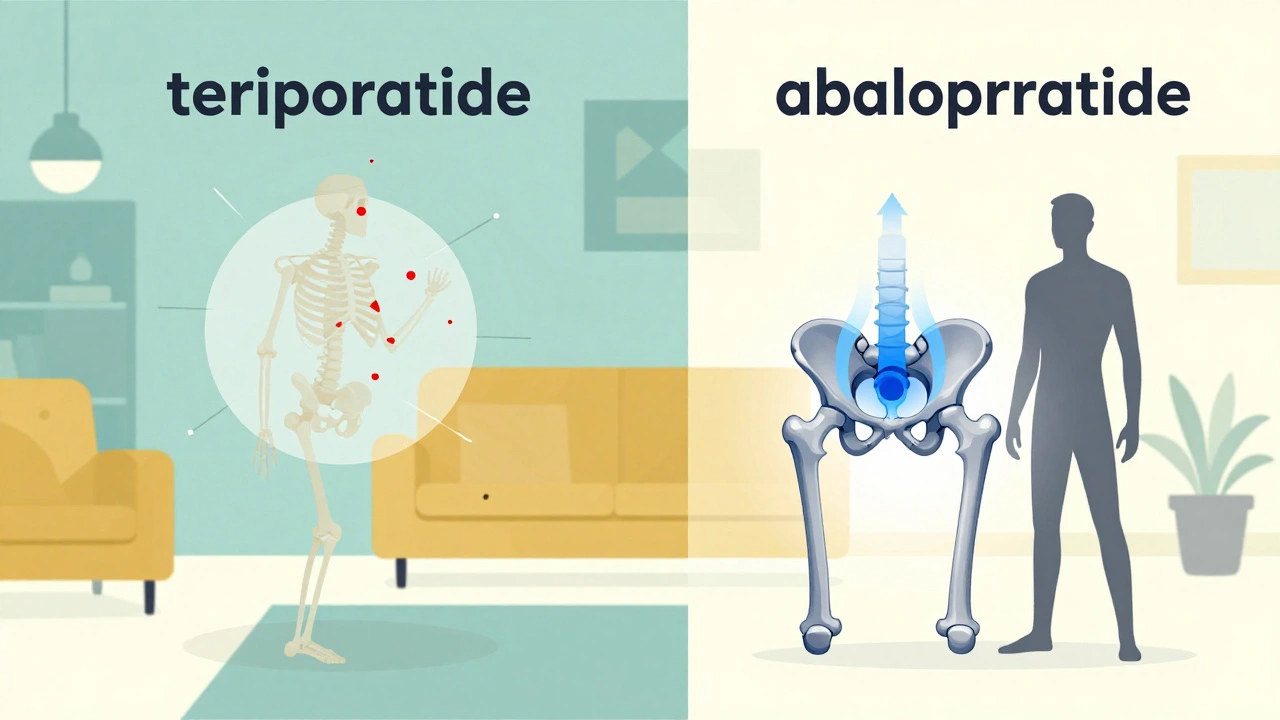
Both drugs mimic parts of natural hormones that tell your bones to grow. Teriparatide is a piece of parathyroid hormone (PTH 1-34). Abaloparatide is a lab-made version of a related hormone called PTHrP. At first glance, they seem similar. But their real difference lies in how they bind to bone cells.
Teriparatide activates multiple pathways in the bone cell receptor, which means it boosts bone formation-but also increases bone breakdown a bit. Abaloparatide is pickier. It locks mainly into the RG shape of the receptor, which favors bone building over breakdown. This small difference leads to bigger results: more bone density in the hip, fewer side effects like high calcium, and better fracture protection in key areas.
Fracture reduction: Which one works better?
In the ACTIVE trial, which tracked over 2,400 postmenopausal women with osteoporosis, abaloparatide cut new spine fractures by more than 90% compared to placebo. Teriparatide did the same, but abaloparatide had a slight edge in preventing non-spine fractures like hip and wrist breaks. A 2024 real-world study of over 43,000 women confirmed this: those on abaloparatide had 17% fewer hip fractures than those on teriparatide. For someone with a T-score below -3.0 in the hip, that difference matters. Your hip is your foundation. If it breaks, your life changes.
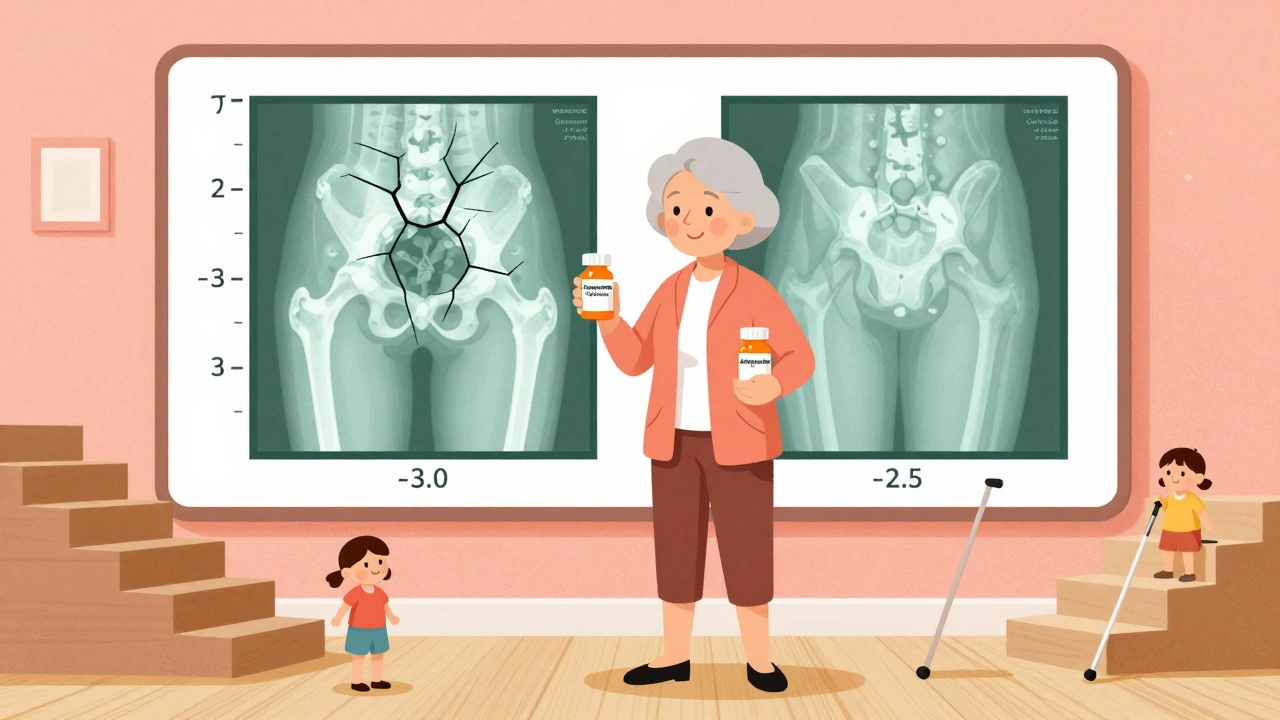
Bone density gains: Numbers that speak volumes
At 18 months, both drugs improved spine bone density by about 9-10%. But the hip? That’s where abaloparatide pulled ahead. In the same trial, abaloparatide boosted hip density by 3.41%, while teriparatide added just 2.04%. That’s a 1.37% difference-enough to push someone from a T-score of -3.0 to -2.5 in most cases. For context, a T-score above -2.5 is no longer classified as osteoporosis. That’s not just a number change. It’s a shift in risk.
And it’s not just about the numbers. A 2025 analysis showed that over half of women starting with a hip T-score as low as -2.7 reached safer levels after 18 months of either drug. But with abaloparatide, the gains were faster and more consistent in the hip, which is often the hardest place to rebuild.
Safety: The hypercalcemia advantage
One of the biggest complaints with teriparatide is high blood calcium-hypercalcemia. In clinical trials, 6.4% of users had it. With abaloparatide? Just 3.4%. That’s nearly half the rate. Why? Because abaloparatide doesn’t overstimulate the parts of the receptor that cause calcium to leak from bone into the blood.
Patients notice this. In patient surveys, 41% of teriparatide users reported dizziness or nausea, often linked to calcium spikes. Only 29% of abaloparatide users did. One Reddit user switched after months of persistent high calcium: “My levels dropped within three months. I didn’t feel like I was walking around with a headache every day.”
Cost and access: The real-world hurdle
Here’s the catch: abaloparatide costs about $5,750 a month. Teriparatide, now available as a generic since early 2024, costs around $4,200. That’s a 30% difference. And insurance? A 2023 analysis found 44% of abaloparatide users faced coverage denials, compared to 28% for teriparatide.
For many, cost decides the outcome. A 65-year-old on a fixed income might choose teriparatide not because it’s better-but because it’s affordable. But if you’re young, active, and have a history of hip fractures, the extra cost might be worth it. The key is to ask your doctor: “Will this drug reduce my chance of breaking my hip? And can I afford it?”
Who gets which drug? Guidelines explained
The American Association of Clinical Endocrinologists (AACE) recommends teriparatide as the first choice for most patients-mostly because it’s been around longer and is cheaper. But they make a clear exception: if your hip T-score is -3.0 or worse, they say go with abaloparatide. Why? Because it builds hip bone faster and reduces hip fractures more.
Other guidelines are less clear-cut. Some doctors still default to teriparatide out of habit. Others, especially those treating high-risk patients, have switched entirely to abaloparatide. The truth? There’s no one-size-fits-all. It depends on your fracture history, your hip density, your budget, and your tolerance for side effects.
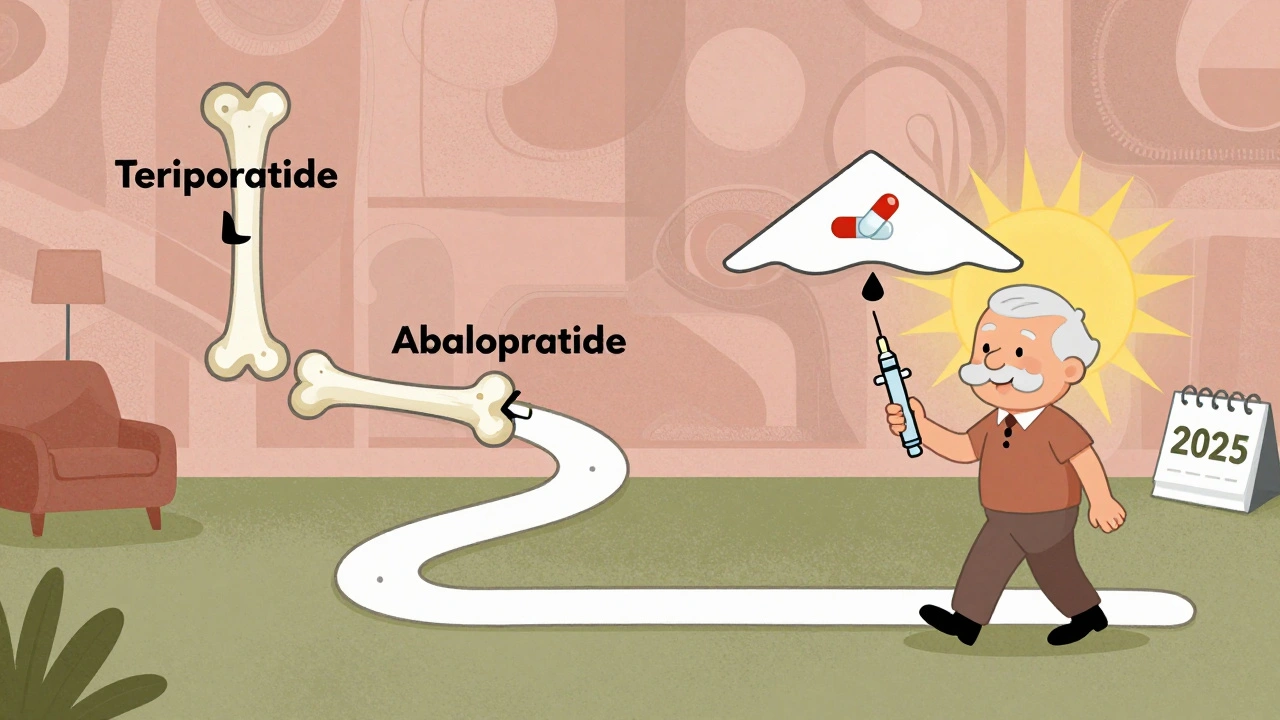
What happens after 18 months?
Neither drug is meant to be taken forever. The FDA limits both to 18-24 months because long-term safety data is still limited. But stopping isn’t the end-it’s the start of the next phase.
The ACTIVE-EXTEND trial showed that if you follow abaloparatide with alendronate (a common bisphosphonate), you keep 68% of your hip bone gains at 3.5 years. Without it? You lose them fast. That’s why doctors now treat these drugs like a one-two punch: build first, then protect.
Same goes for teriparatide. After 18 months, switching to an antiresorptive drug isn’t optional-it’s essential. Skipping this step is like building a house and then forgetting to install the roof.
Real patient experiences: What users say
On patient forums, stories vary. One user, “FractureFree88,” said teriparatide gave her a 12.3% spine boost-better than abaloparatide’s 9.8%. But she quit after three months because of dizziness. Another, “BoneWarrior42,” switched from teriparatide to abaloparatide after hypercalcemia kept coming back. “I felt like myself again,” she wrote.
Discontinuation rates tell their own story. In a 2024 survey of over 1,200 patients, 32% stopped teriparatide within a year. Only 24% stopped abaloparatide. The main reason? Side effects. Not the injection. Not the cost. The way it made them feel.
The future: Weekly shots and longer use
Right now, both drugs require a daily injection. That’s hard to stick with. But Radius Health is testing a weekly version of abaloparatide. Phase 3 trials ended in late 2023, and results are expected in mid-2025. If it works, adherence could jump from 60% to 85%.
Also, the FDA is pushing for longer treatment windows. Right now, we’re limited to two years. But new data suggests that with careful monitoring, extending use beyond 24 months might be safe and effective-especially for people who still have very low bone density after the first course.
What to ask your doctor
- What’s my hip T-score? If it’s below -3.0, abaloparatide may be the better choice.
- Have I had a nonvertebral fracture? If yes, abaloparatide has stronger evidence for preventing the next one.
- Can I afford this? Ask about patient assistance programs. Both manufacturers offer them.
- Will I be switched to a maintenance drug after 18 months? If not, ask why.
- What are my chances of high calcium? If I’ve had it before, abaloparatide is safer.
Final thoughts: It’s not about which is best-it’s about which is right for you
Teriparatide and abaloparatide aren’t rivals. They’re tools. One is tried and true, cheaper, and widely available. The other is newer, more precise, and better for the hip. Neither is perfect. Both require commitment. But for someone with severe osteoporosis, either one can mean the difference between a fall and a fracture-and a fracture and a lifetime of pain.
The goal isn’t just to raise a number on a scan. It’s to let you walk without fear. To climb stairs. To hold your grandchild. To live without waiting for the next break. That’s what these drugs do. And choosing between them isn’t about science alone. It’s about your life, your body, and what you’re willing to do to protect it.

Andrea Petrov
December 8, 2025 AT 14:51And why is teriparatide cheaper? Because it's old. And old drugs are easier to manipulate. The real reason they're pushing abaloparatide? It's patented. And patents mean profit. Not health.
Suzanne Johnston
December 8, 2025 AT 19:15Maybe the real question isn't which drug builds bone faster-but which one lets you live without fear. And that's not a number. It's a feeling.
Graham Abbas
December 9, 2025 AT 17:33And don't even get me started on the cost. $5,750 a month? That's a luxury car payment. But if you're a 68-year-old widow who just broke her hip falling out of bed, you don't care about the price tag-you care about not dying in a hospital bed because your insurance denied coverage.
They call this medicine. I call it a moral dilemma wrapped in a syringe.
George Taylor
December 11, 2025 AT 00:43Meanwhile, I'm just doing yoga and eating kale. My T-score went from -2.9 to -2.6 in 10 months. No needles. No side effects. No $5,750/month.
Also, the word 'abaloparatide' is 12 letters. That's too many. It's a scam.
Chris Marel
December 11, 2025 AT 01:15I just wanted to say thank you for writing this so clearly. Most medical stuff is written like a legal contract. This felt like someone sitting across from me, explaining it like we're both trying to understand the same puzzle.
Can I ask-do you know if any NGOs or charities help with access to these drugs in low-income countries? I'd love to help her get the best shot, even if it's not the one she can afford.
William Umstattd
December 11, 2025 AT 04:23Let me remind you: the ACTIVE trial was funded by Radius Health. The 2024 real-world study? Sponsored by the same company that makes abaloparatide.
And you're quoting T-scores like they're gospel. T-scores are statistical estimates. They're not truth. They're projections based on a sample of mostly white, postmenopausal women in the U.S.
And you're not even talking about the fact that both drugs are contraindicated in patients with Paget’s disease, bone metastases, or prior radiation. But you're too busy debating which one is 'better' to notice that neither is safe for half the population.
Wake up. This isn't science. It's marketing dressed in lab coats.
Elliot Barrett
December 12, 2025 AT 02:12So now she's on abaloparatide. And guess what? Her calcium is normal. She sleeps. She doesn't feel like she's got a battery in her skull.
Stop overcomplicating it. If one drug makes you feel like death and the other lets you breathe? Choose the one that doesn't turn your body into a hostile environment.
And stop pretending cost is the only barrier. It's not. It's the side effects. And no one talks about that enough.
Maria Elisha
December 13, 2025 AT 12:21Also, the cost? Yeah, it's insane. But my insurance covered it because I had a vertebral fracture. If you haven't broken a bone yet, you probably don't qualify. So stop acting like everyone's got access to this. Most people just take calcium and hope.
iswarya bala
December 13, 2025 AT 13:55Stacy Tolbert
December 14, 2025 AT 07:04My husband says I’m being dramatic. But he doesn’t see me at 3 a.m., staring at the ceiling, wondering if I’ll be able to hold my granddaughter next year.
So yeah. The cost is high. The side effects are real. But the fear? That’s the heaviest thing of all.
Ryan Brady
December 16, 2025 AT 04:42Also, 18 months? That’s too long. I can’t even stick to a vitamin routine. Who’s gonna jab themselves daily for over a year?
Just eat more milk. Problem solved. 💪🥛
Raja Herbal
December 18, 2025 AT 00:06It's not about bone density. It's about class. The rich get precision medicine. The rest get the generic version that makes them dizzy.
And yet, we're all supposed to be grateful for the 'progress.'
How poetic.