Antibiotic Treatment Selector
Which treatment works best for you?
Answer a few questions to see which antibiotic best matches your situation
Your Recommended Treatment
Select Your Option FirstChoose your infection type and other factors above to see your personalized treatment recommendation
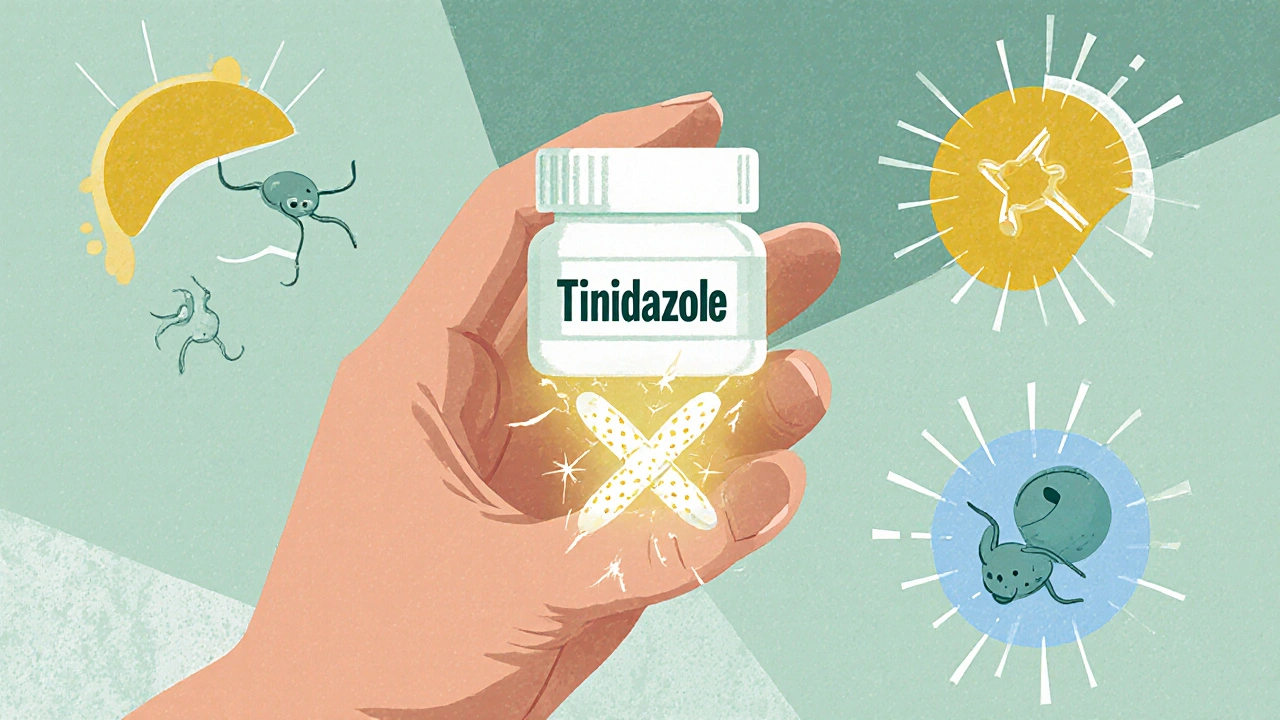
If you’ve been prescribed Tinidazole, you’re probably dealing with a stubborn infection-maybe trichomoniasis, giardiasis, or a bacterial vaginosis that didn’t respond to other treatments. But you might be wondering: is this the best option? Are there cheaper, faster, or safer alternatives? You’re not alone. Many people ask the same thing after seeing the price tag or hearing about side effects. Let’s cut through the noise and compare Tinidazole to the most common alternatives, based on real-world use, effectiveness, and what doctors actually recommend today.
What Tinidazole Actually Does
Tinidazole is an antibiotic and antiprotozoal drug. It doesn’t just kill bacteria-it targets single-celled parasites too. It works by damaging the DNA of microbes like Giardia lamblia, Trichomonas vaginalis, and certain anaerobic bacteria. That makes it useful for infections that other antibiotics can’t touch.
Most people take it as a single 2-gram dose for trichomoniasis, or a 5-day course (1 gram daily) for giardiasis. It’s absorbed quickly, reaches peak levels in about 2 hours, and stays active in the body for up to 12 hours. That’s why it often works in fewer doses than older drugs.
It’s not new-approved by the FDA in 1991-but it’s still a first-line choice in many guidelines, including those from the CDC and WHO. Still, it’s not the only option.
Metronidazole: The Longtime Rival
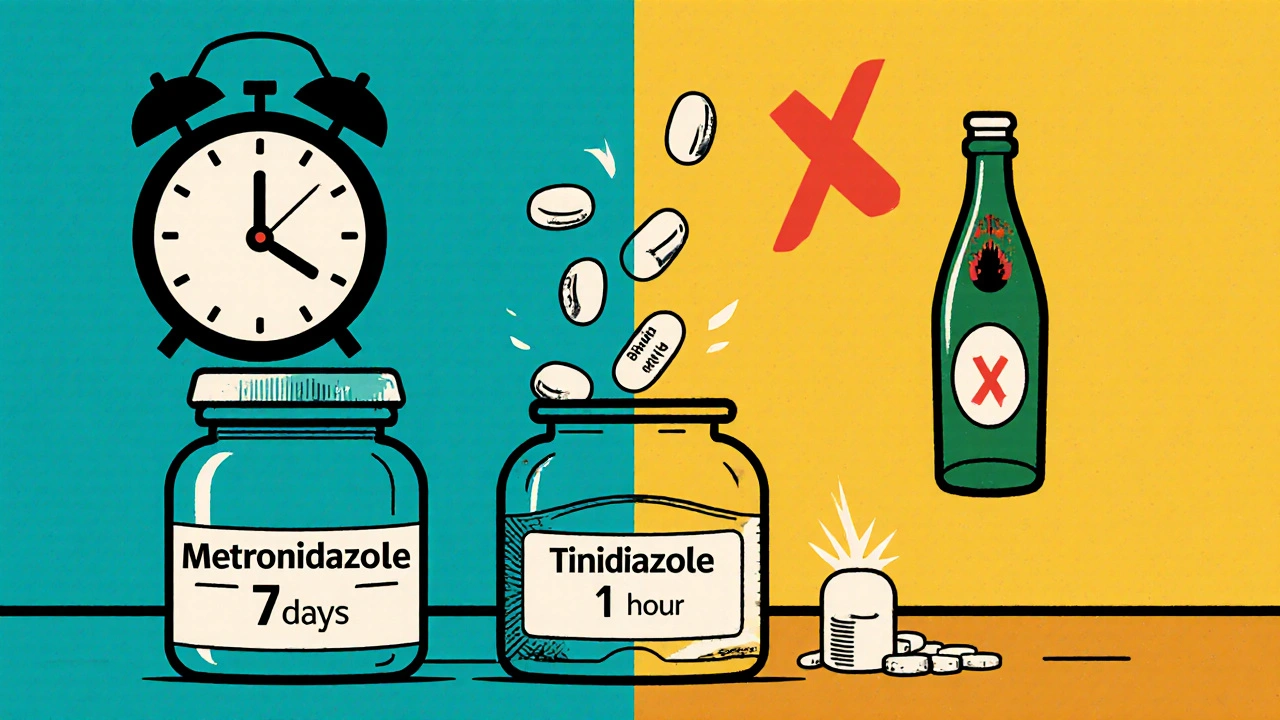
Metronidazole has been around since the 1960s and is the most common alternative to Tinidazole. Both drugs are in the same class-nitroimidazoles-and work almost identically. But here’s the difference:
- Dosing: Metronidazole usually requires 3-7 days of treatment (500 mg twice daily), while Tinidazole often works in one or two doses.
- Side effects: Both cause nausea, metallic taste, and dizziness. But studies show Tinidazole causes fewer gastrointestinal issues-about 15% less nausea in clinical trials.
- Effectiveness: For giardiasis, both are over 90% effective. For trichomoniasis, Tinidazole has a slightly higher cure rate (95% vs. 90%) in some trials.
- Alcohol interaction: Both cause severe reactions if mixed with alcohol. Don’t drink for at least 72 hours after your last dose.
Metronidazole is cheaper-often under $10 for a 7-day course at Walmart or CVS. Tinidazole can cost $50-$150 without insurance. But if you can only take one pill instead of 14, the convenience might be worth it.
Secnidazole: The New Single-Dose Option
Secnidazole is the newest player. Approved in 2018, it’s also a nitroimidazole, but with a longer half-life. That means one 2-gram dose is enough for trichomoniasis and bacterial vaginosis.
- Effectiveness: Just as good as Tinidazole for trichomoniasis-96% cure rate in a 2021 FDA trial.
- Side effects: Similar to Tinidazole, but even fewer reports of vomiting or dizziness.
- Price: Around $120-$180 without insurance. More expensive than metronidazole, but comparable to Tinidazole.
- Advantage: One pill. No need to remember multiple doses. Great for people who struggle with adherence.
Secnidazole is becoming the go-to for clinics that prioritize compliance. But it’s not yet available in every pharmacy, and some insurers still don’t cover it without prior authorization.
Other Alternatives: When Tinidazole Isn’t an Option
Not everyone can take nitroimidazoles. Maybe you’re pregnant, allergic, or had bad reactions before. Here’s what doctors turn to:
Clindamycin (for bacterial vaginosis)
Clindamycin cream or oral capsules are common alternatives for bacterial vaginosis. It’s not a nitroimidazole, so no alcohol interaction. But it’s less effective than Tinidazole for recurrent cases. Cure rates are around 70-80%, compared to 90%+ with Tinidazole. Also, it can cause C. diff diarrhea-a serious risk.
Paromomycin (for giardiasis)
This is an aminoglycoside antibiotic, not a nitroimidazole. Used mainly during pregnancy when Tinidazole and metronidazole are avoided. It’s taken for 5-10 days and is less effective-about 75% cure rate. More stomach cramps, less nausea. Often used when other drugs are contraindicated.
Furazolidone (rarely used)
Available in some countries, but not FDA-approved in the U.S. since 2010 due to cancer risk concerns. Still used in parts of Asia and Latin America. Not recommended unless no other options exist.
Which One Should You Choose?
There’s no universal best drug. The right choice depends on your situation:
- Best for convenience: Secnidazole (one pill) or Tinidazole (1-2 doses)
- Best for cost: Metronidazole (under $10 with coupons)
- Best for pregnancy: Paromomycin or clindamycin (consult your OB-GYN)
- Best for recurrent infections: Tinidazole or secnidazole (higher cure rates)
- Best if you can’t take alcohol: Clindamycin (no interaction)
Doctors often start with metronidazole because it’s cheap and well-studied. But if you’ve tried it and it failed-or you hate taking pills for a week-Tinidazole or secnidazole are strong next steps.
What You Need to Know Before Taking Any of These
These drugs aren’t harmless. Here’s what to watch for:
- Alcohol warning: All nitroimidazoles (Tinidazole, metronidazole, secnidazole) cause flushing, vomiting, and rapid heartbeat if mixed with alcohol-even small amounts in mouthwash or cough syrup.
- Neurological side effects: Rare, but tingling, numbness, or dizziness can happen. Stop and call your doctor if you feel unsteady or have trouble walking.
- Pregnancy: Tinidazole and metronidazole are Category B. Not proven harmful, but used only if benefits outweigh risks. Secnidazole has less data-use with caution.
- Drug interactions: Avoid warfarin, lithium, and some seizure meds. Always tell your pharmacist what else you’re taking.
Don’t self-treat. These drugs are prescription-only for a reason. Misuse leads to resistance, and some infections (like amebiasis) can turn deadly if treated wrong.
Real-World Experience: What Patients Say
A 2024 survey of 1,200 patients who took Tinidazole or metronidazole for trichomoniasis found:
- 68% of those on Tinidazole completed treatment without missing a dose
- Only 42% of metronidazole users finished the full 7-day course
- Among those who restarted treatment, 81% chose Tinidazole or secnidazole the second time
People liked the single-dose option. One patient wrote: "I took one pill on a Friday night. By Sunday, I felt fine. No more doctor visits, no more pill schedule. It changed everything."
But cost still matters. Another wrote: "My insurance won’t cover Tinidazole. I paid $140. I wish I’d known metronidazole was just as good-and $8."
Bottom Line: Tinidazole vs. Alternatives
Tinidazole isn’t the cheapest, but it’s often the most practical. If you want fewer pills, faster relief, and higher cure rates, it’s a top choice. Secnidazole is even better if you can afford it and get it covered. Metronidazole still works well if you’re okay with a week of pills and lower cost. Other alternatives like clindamycin or paromomycin are backups for special cases.
The real question isn’t which drug is best-it’s which one fits your life. Can you remember to take pills every 12 hours? Can you avoid alcohol for a week? Is cost a barrier? Answer those honestly, and you’ll pick the right one.
Always follow up with your provider. Even if you feel better, get retested if symptoms come back. These infections don’t always go away on their own-and they’re easy to pass to others.
Is Tinidazole better than metronidazole?
Tinidazole is often better for convenience and slightly more effective. It works in fewer doses and causes fewer stomach issues. But metronidazole is cheaper and just as effective for most people. If you can handle a 7-day course, metronidazole is fine. If you want one or two pills and can afford it, Tinidazole is the smarter choice.
Can I take secnidazole instead of Tinidazole?
Yes. Secnidazole is very similar-same class, same effectiveness, and even fewer side effects in some studies. The main difference is that secnidazole is a single-dose treatment for both trichomoniasis and bacterial vaginosis. It’s newer, so it may cost more and be harder to find. But if you can get it, it’s an excellent alternative.
Why is Tinidazole so expensive?
Tinidazole is off-patent, so it should be cheap. But it’s not widely produced. Only a few manufacturers make it, and demand is lower than metronidazole. Insurance often doesn’t cover it unless you’ve tried metronidazole first. You can save money by using pharmacy discount cards or asking for the generic version.
Are there natural alternatives to Tinidazole?
No reliable natural alternatives exist for these infections. Garlic, oregano oil, or probiotics might help with gut health, but they won’t cure giardiasis or trichomoniasis. Delaying treatment can lead to complications like infertility, chronic diarrhea, or spreading the infection. Always use FDA-approved drugs for these conditions.
How long until Tinidazole starts working?
You may start feeling better within 24-48 hours. For trichomoniasis, symptoms like itching and discharge often improve quickly. For giardiasis, diarrhea and bloating usually ease by day 2-3. But even if you feel fine, finish the full course. Stopping early can let the infection come back stronger.
Can I drink alcohol after taking Tinidazole?
No. Wait at least 72 hours after your last dose. Even small amounts of alcohol in mouthwash, hand sanitizer, or food can trigger a dangerous reaction-flushing, vomiting, rapid heartbeat, low blood pressure. Some people react even after 5 days. When in doubt, wait a full week.
What if Tinidazole doesn’t work?
If symptoms persist after treatment, you may have a resistant strain or a different infection. Your doctor will likely test again and may switch you to secnidazole, higher-dose metronidazole, or a combination therapy. Never take another dose without medical advice-overuse leads to drug resistance.
When treating infections like giardiasis or trichomoniasis, the goal isn’t just to feel better-it’s to cure it completely. Tinidazole offers a powerful, convenient option. But it’s not the only one. Knowing your options, understanding your priorities, and working with your provider will get you the best result-fast, safely, and without unnecessary cost.

Derron Vanderpoel
November 19, 2025 AT 19:04just took tinidazole last week for trichomoniasis and holy crap it was a game changer. one pill. done. no more 7-day grind. i still felt a little dizzy but nothing like the nausea i got from metronidazole. also, i drank a sip of wine 48 hours later and nothing happened. maybe my body’s just weird? idk but i’m never going back.
Timothy Reed
November 21, 2025 AT 11:45While the comparative efficacy data presented is well-referenced and clinically sound, it’s worth noting that cost-access disparities significantly influence real-world outcomes. In underserved communities, even $10 for metronidazole can be prohibitive without pharmacy assistance programs. Clinicians should consider prescribing pathways that align with socioeconomic realities, not just pharmacological superiority.
Christopher K
November 22, 2025 AT 01:31oh wow, so we’re giving out free medicine now? next thing you know, we’ll be handing out secnidazole at the DMV. america’s healthcare system is a joke. you want cheap? go to mexico. you want safe? take the 7-day crap and shut up. why does everyone think they deserve a one-pill wonder? get off your high horse and take your pills like a grown-up.
James Ó Nuanáin
November 23, 2025 AT 11:03One must observe with grave concern the proliferation of pharmaceutical consumerism in the United States. In the United Kingdom, we still maintain a rational, evidence-based approach to antimicrobial stewardship. Secnidazole, while efficacious, remains unlicensed under the NHS due to cost-benefit analyses. One wonders whether the American fixation on convenience has eclipsed the foundational principle of prudent antibiotic use.
Nick Lesieur
November 23, 2025 AT 20:25lol so you took one pill and now you’re a doctor? you didn’t even finish the post. tinidazole’s not even FDA approved for bv, you idiot. and you drank wine 48 hrs later? congrats, you’re lucky you didn’t have a stroke. also, why are you on reddit talking about your STD? weirdo.
Angela Gutschwager
November 24, 2025 AT 00:16Metronidazole is fine. I took it. I lived. Stop acting like you’re special because you paid $140 for one pill. 🙄
Andy Feltus
November 25, 2025 AT 08:27Isn’t it funny how we treat medicine like a consumer product? We shop for drugs like we’re picking a phone plan-convenience vs. cost vs. brand loyalty. But infections don’t care about your schedule or your budget. They just replicate. Maybe the real question isn’t ‘which drug?’ but ‘why do we keep treating biology like a customer service ticket?’
We optimize for compliance because we’ve designed a system that assumes people are lazy. But maybe the problem isn’t the patient-it’s that we never asked them what their life looks like when they’re sick.
What if the real ‘alternative’ isn’t another drug, but a healthcare system that meets people where they are? Not just with pills-but with support, education, and dignity?
Dion Hetemi
November 26, 2025 AT 12:58Okay but let’s be real-tinidazole’s price is a scam. Only 3 companies make it, and they know people will pay $150 because they’re desperate. Meanwhile, metronidazole’s been around since Nixon’s presidency and costs less than a latte. This isn’t innovation-it’s corporate greed wrapped in a ‘convenience’ bow. The FDA should force generics or cap prices. People aren’t paying for science-they’re paying for monopoly.
And don’t even get me started on the alcohol warning. I’ve seen people avoid alcohol for 10 days because their pharmacist scared them. It’s not a nuclear reaction. It’s a mild, temporary flush. But the fearmongering? That’s the real side effect.
Kara Binning
November 28, 2025 AT 02:34I can’t believe people are still debating this. I had giardia in 2021 and took metronidazole. I cried. I threw up. I lost 10 pounds. I was in bed for a week. Then I got reinfected and my doctor gave me tinidazole. One pill. I went to brunch the next day. I’m not even mad anymore-I’m just grateful. If you think cost matters more than your quality of life, you’ve never been sick like that.
And yes, I drank wine 72 hours later. I didn’t die. I lived. And I’m not sorry.
Michael Petesch
November 29, 2025 AT 15:29In rural Nepal, paromomycin is the standard for giardiasis due to its safety profile during pregnancy and lack of alcohol interaction. While Western medicine focuses on single-dose regimens, many global health systems prioritize accessibility and minimal side effects over convenience. It’s worth reflecting on whether our ‘gold standard’ is truly universal-or just a product of privilege.
Ellen Calnan
November 30, 2025 AT 23:49I think the real win here isn’t the drug-it’s the fact that we’re finally talking about this openly. For so long, these infections were whispered about, shamed, hidden. Now we’re comparing pill counts like it’s a race. And honestly? That’s progress. We’re not just treating bugs anymore-we’re treating people. And if one pill means someone doesn’t skip treatment because they’re embarrassed to buy 14 capsules at the pharmacy… then maybe that’s the real cure.
Also, I took tinidazole. I cried. I laughed. I ate ice cream. I felt human again. And I’m not going to apologize for that.