Anticholinergic Cognitive Burden (ACB) Score Calculator
Medication Risk Calculator
This tool calculates your Anticholinergic Cognitive Burden (ACB) score based on medications you're taking. Scores of 3 or higher indicate increased risk of cognitive decline and other serious side effects.
Current Medications
Your Anticholinergic Risk
Your ACB Score:
0
Combining tricyclic antidepressants (TCAs) with first-generation antihistamines might seem like a simple fix - one for depression, another for allergies or sleep. But what looks like a routine prescription can quietly push your body into a dangerous state called anticholinergic overload. This isn’t a rare edge case. It’s happening right now in homes, clinics, and hospitals - especially among older adults - and many doctors still don’t see it coming.
What Exactly Is Anticholinergic Overload?
Your body uses a chemical called acetylcholine to keep things running smoothly: memory, digestion, bladder control, heart rate, even how alert you feel. Anticholinergic drugs block this chemical. Individually, a low dose of a TCA or an antihistamine might cause mild dry mouth or drowsiness. But when you stack them? The effects multiply. It’s like turning up the volume on a faulty speaker - the signal gets distorted, and eventually, it breaks.Take amitriptyline (Elavil), one of the most common TCAs. It blocks acetylcholine receptors with high strength. Now add diphenhydramine (Benadryl), a go-to sleep aid or allergy pill. Diphenhydramine isn’t as strong per milligram, but people take it in higher doses - 25 to 50 mg, multiple times a day. Together, they overwhelm the system. The result? Confusion, blurred vision, constipation, urinary retention, rapid heartbeat, and in severe cases, full-blown delirium.
Why This Combo Is So Dangerous for Older Adults
Your liver and kidneys don’t work as fast after age 65. That means drugs stick around longer. A 70-year-old taking amitriptyline for nerve pain and diphenhydramine for insomnia isn’t just doubling up on side effects - they’re stacking up a toxic load. A 2015 JAMA Internal Medicine study found that people who took high-anticholinergic drugs for just three years had a 54% higher risk of developing dementia. That’s not speculation. That’s data from over 3,400 people tracked for 10 years.And it’s not just dementia. The American Geriatrics Society’s Beers Criteria (2023 update) explicitly warns: “First-generation antihistamines should be avoided in older adults taking TCAs.” Yet, a 2021 survey of pharmacists showed that nearly 3 in 10 anticholinergic overload cases they saw came from exactly this combo. One patient in Manchester, UK, ended up in the ER after his GP added Benadryl to his amitriptyline for sleep. He couldn’t urinate. His mind went foggy. He didn’t recognize his own daughter. That’s anticholinergic delirium - and it’s reversible if caught early.
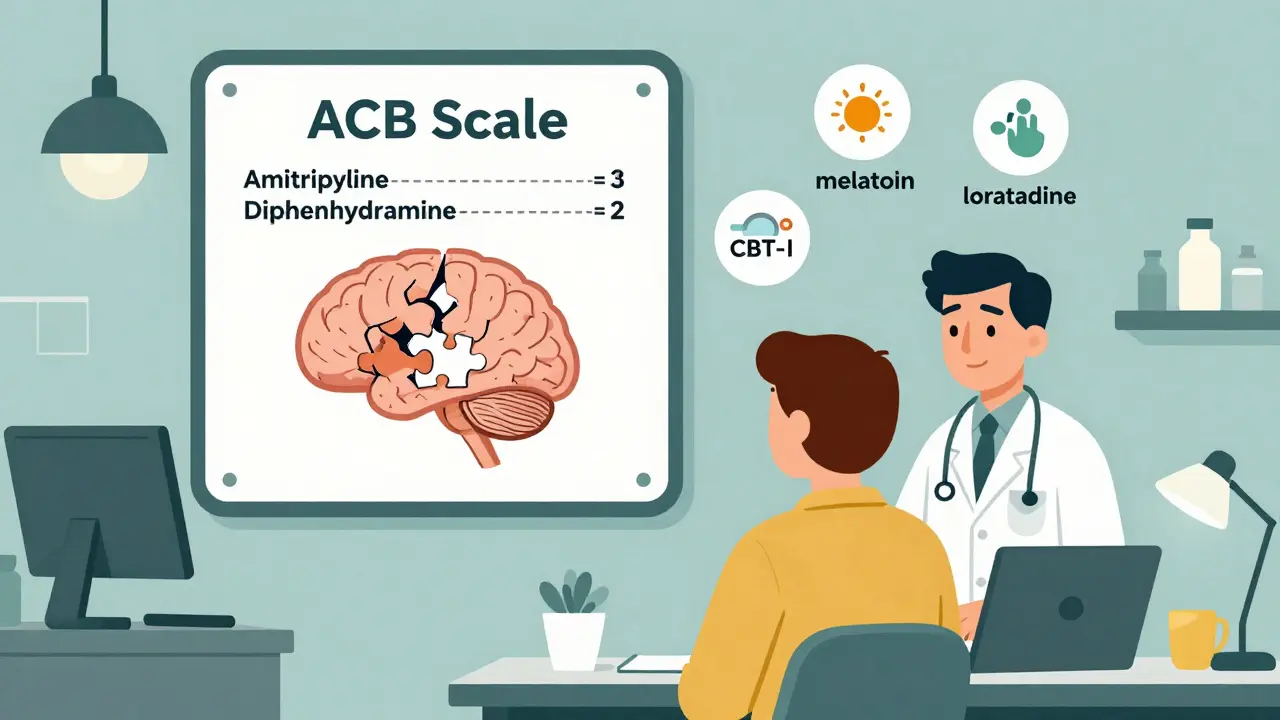
How Much Is Too Much? The ACB Scale Explained
Clinicians now use the Anticholinergic Cognitive Burden (ACB) scale to measure risk. It’s simple: each drug gets a score.- Amitriptyline = 3 (highest risk)
- Diphenhydramine = 2
- Hydroxyzine = 2
- Loratadine (Claritin) = 0
- Fexofenadine (Allegra) = 0
When you add them up, a score of 3 or more over time increases dementia risk. A score of 5 - like amitriptyline + diphenhydramine - doubles it. That’s why electronic health records now flag these combinations. Epic, one of the biggest EHR systems, blocks the prescription 92% of the time. But not all clinics have those alerts. And many patients still get these prescriptions because the doctor doesn’t know the score.
Not All Antidepressants Are Created Equal
TCAs aren’t all the same. Some have much lower anticholinergic effects. Nortriptyline and desipramine are far safer choices if you need a TCA. Clomipramine is powerful for OCD and chronic pain, but it’s still high-risk. Meanwhile, SSRIs like sertraline or escitalopram have anticholinergic side effects in only 5-10% of users - compared to 30-50% with TCAs.So why are TCAs still used? Because they work. For neuropathic pain, fibromyalgia, or severe depression that doesn’t respond to SSRIs, TCAs are still first-line. But that doesn’t mean you need to pair them with antihistamines. There are better ways.
What About Sleep? There Are Safer Alternatives
Many people take diphenhydramine because it’s cheap, over-the-counter, and makes them sleepy. But it’s not a sleep aid - it’s a sedative. It doesn’t improve sleep quality. It just knocks you out. And it lingers in your system. One night of it can leave you groggy the next day. For older adults, that’s a fall risk.Try these instead:
- Melatonin (0.5-5 mg) - natural, low-risk, helps reset your body clock
- Mirtazapine (low dose) - an antidepressant with mild sedative effects, but lower anticholinergic burden than TCAs
- Cognitive behavioral therapy for insomnia (CBT-I) - proven, long-lasting results without drugs
One patient in Manchester switched from amitriptyline + Benadryl to melatonin + CBT-I. Within six weeks, his sleep improved, his confusion cleared, and his bladder function returned to normal. No ER visit. No hospital stay.
What to Do If You’re Taking This Combo
If you’re on a TCA and an antihistamine, here’s what to do now:- Check your meds. Look up each drug on the ACB scale. If your total is 3 or higher, talk to your doctor.
- Ask if you can switch to a second-generation antihistamine: loratadine, cetirizine, or fexofenadine. They don’t block acetylcholine.
- If you’re taking diphenhydramine for sleep, ask about melatonin or non-drug options.
- Request a cognitive check. Ask your doctor to run a Mini-Mental State Examination (MMSE). A score below 24 could mean anticholinergic toxicity.
- Don’t stop cold turkey. TCAs need to be tapered. Antihistamines can be switched immediately.
The Bigger Picture: Why This Keeps Happening
The problem isn’t just ignorance. It’s system failure. TCAs are old drugs. Antihistamines are OTC. Neither gets the same scrutiny as newer medications. Prescribers assume “it’s safe because it’s been around forever.” But we now know better. A 2023 FDA requirement forced all TCA and first-gen antihistamine labels to include warnings about cumulative anticholinergic effects. That’s progress.And it’s working. A 2023 study in the Journal of the American Geriatrics Society showed that when pharmacists actively reviewed prescriptions and helped deprescribe anticholinergics, patients’ cognitive scores improved by 34% in 18 months. In one UK health system, 41% of dangerous TCA-antihistamine pairs were stopped after an audit. That’s not luck. That’s intervention.
Final Thought: You Don’t Have to Accept This Risk
You might be told, “This is the best we can do.” But that’s outdated thinking. Better options exist. Safer combinations are available. And your brain deserves protection - not just from depression, but from preventable drug damage.If you’re taking a TCA and an antihistamine, don’t wait for confusion to set in. Talk to your doctor today. Ask for the ACB score. Ask for alternatives. Your future self will thank you.
Can I take Benadryl with amitriptyline?
No, combining Benadryl (diphenhydramine) with amitriptyline significantly increases the risk of anticholinergic overload. Both drugs block acetylcholine, and together they can cause confusion, urinary retention, rapid heartbeat, and delirium - especially in people over 65. Even if you’ve taken them together for years, the risk builds over time. Switch to a non-anticholinergic sleep aid like melatonin or a second-generation antihistamine like loratadine.
Are all antihistamines dangerous with TCAs?
No. Only first-generation antihistamines like diphenhydramine, hydroxyzine, and chlorpheniramine have strong anticholinergic effects. Second-generation antihistamines - such as loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) - have minimal to no effect on acetylcholine receptors and are much safer to use with TCAs. Always check the active ingredient, not just the brand name.
How do I know if I’m experiencing anticholinergic overload?
Watch for these signs: sudden confusion or memory lapses, trouble urinating, dry mouth and eyes, blurred vision, constipation, fast heartbeat, dizziness, or feeling unusually sleepy. If you notice these after starting or increasing either drug, contact your doctor immediately. A simple Mini-Mental State Examination (MMSE) can confirm if cognitive decline is drug-related. Scores below 24 suggest anticholinergic toxicity.
Why are TCAs still prescribed if they’re so risky?
TCAs like amitriptyline are still used because they work well for specific conditions - especially nerve pain, fibromyalgia, and treatment-resistant depression. They’re also cheaper than newer drugs. But they’re not first-line for everyone. For most people with depression, SSRIs are safer. TCAs should only be chosen when other options fail, and even then, they should be paired with low-risk medications, not antihistamines.
Can anticholinergic damage be reversed?
Yes - if caught early. Cognitive decline from anticholinergic overload often improves within weeks after stopping the drugs. A 2023 study showed that deprescribing these medications led to a 34% improvement in memory and thinking skills over 18 months. But the longer you’re exposed, the harder it is to recover. That’s why early detection matters. Don’t wait for dementia to develop before acting.

