Antibiotic Resistance: What It Is and How It's Changing How We Treat Infections
When bacteria stop responding to antibiotics, that’s antibiotic resistance, the ability of bacteria to survive and multiply despite treatment with drugs designed to kill them. Also known as drug-resistant bacteria, it’s not a future threat—it’s happening right now, making simple infections like urinary tract infections or pneumonia harder to treat and sometimes deadly. Every time you take an antibiotic when you don’t need it, or don’t finish the full course, you’re helping these bacteria adapt. They don’t become immune—they evolve. And the more we use these drugs, the faster they change.
This isn’t just about taking pills wrong. antibiotic misuse, including using leftover antibiotics or taking them for viral infections like colds or flu is a huge driver. Even in hospitals, overprescribing and broad-spectrum antibiotics used as a default are pushing resistant strains into the wild. superbugs, bacteria like MRSA or drug-resistant E. coli that no longer respond to standard treatments are showing up in nursing homes, gyms, and even grocery stores. You don’t need to be sick to be at risk—just being near someone who’s been treated with antibiotics can expose you to these tough strains.
And it’s not just about the drugs themselves. antibiotic side effects, like yeast infections or gut imbalance from killing off good bacteria are common, and they’re why so many people stop taking their meds early. That’s exactly when the strongest bacteria survive and multiply. Some people turn to herbal remedies or skip treatment altogether, which only makes things worse. But there are smarter ways: using narrow-spectrum antibiotics only when needed, testing to confirm bacterial infections before prescribing, and using probiotics to protect your microbiome.
What you’ll find in these articles isn’t just theory—it’s real-world guidance. You’ll learn how antibiotics trigger yeast infections, why generic versions work just as well, how to spot fake meds, and what alternatives exist when standard drugs fail. There’s a post on Tinidazole vs. metronidazole for stubborn infections, another on Cepmox (amoxicillin) and when it’s actually needed, and one on how to prevent yeast infections after antibiotics. You’ll also see how drug interactions, like mixing antibiotics with supplements, can make things worse—or better. These aren’t abstract ideas. They’re tools you can use today to protect yourself and your family from the growing threat of antibiotic resistance.
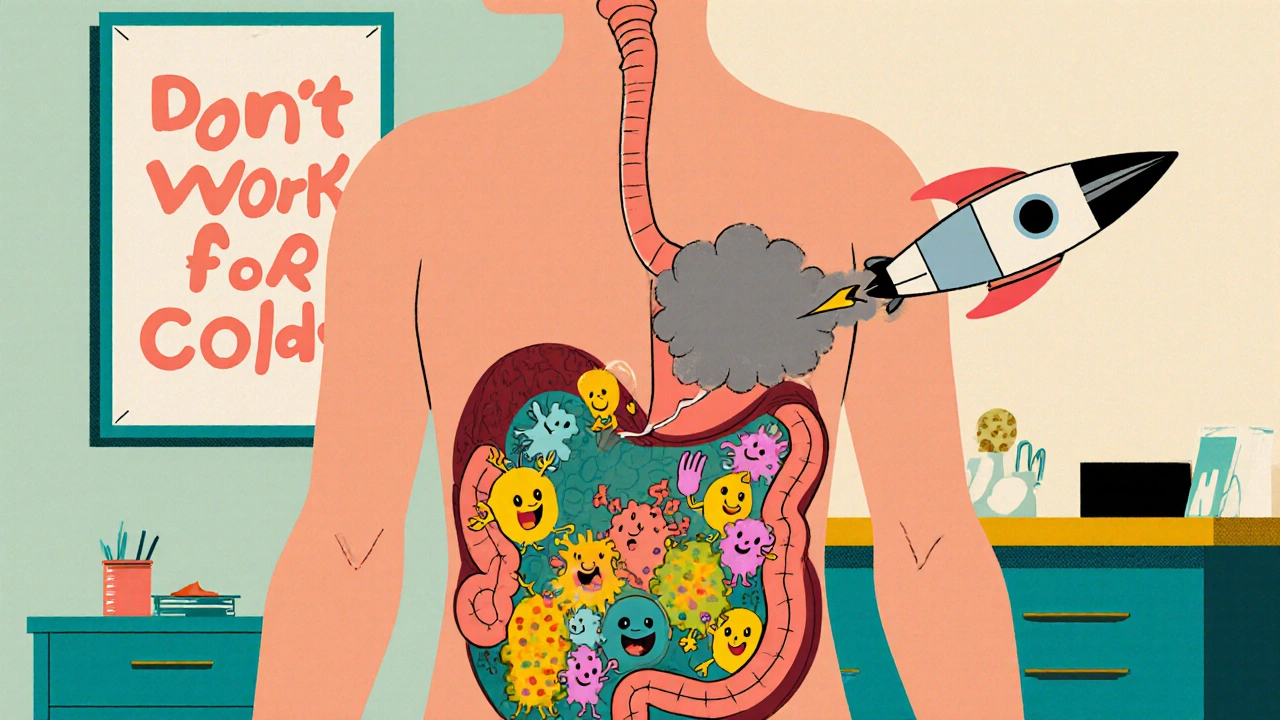
Antibiotic Stewardship: How Smart Prescribing Stops Resistance and Saves Your Gut
Antibiotic stewardship means using antibiotics only when needed and in the right way. It stops resistance, prevents deadly gut infections like C. diff, and saves lives. Learn how smarter prescribing protects your health.
