Brand-Name Drugs: What They Are, How They Compare to Generics, and What You Need to Know
When you hear brand-name drugs, original medications developed and marketed by pharmaceutical companies under a patent-protected name. Also known as proprietary drugs, they’re the first version of a medicine to hit the market after years of research and testing. These are the pills and patches you see advertised on TV—like Viagra, Nolvadex, or Tylenol. But behind every brand-name drug is a chemical formula that eventually becomes available as a cheaper copy. That’s where generic medications, chemically identical versions of brand-name drugs sold after the patent expires come in. They work the same way, have the same side effects, and are held to the same safety standards. The only real difference? Price—and sometimes, the color of the pill.
So why do brand-name drugs cost so much more? It’s not because they’re better. It’s because the company that made them spent millions developing the drug, running clinical trials, and getting FDA approval. Once that patent runs out—usually after 10 to 12 years—other companies can make the same drug without repeating all that work. That’s when generics appear, often at 80% less cost. You’ll see this pattern in posts about generic Premarin, the estrogen replacement therapy now available as a low-cost alternative, or generic Motrin, the cheaper version of ibuprofen that works just as well. Even Fildena XXX, a generic version of sildenafil sold for erectile dysfunction, follows this exact model. People aren’t paying for better science—they’re paying for the brand.
But here’s the thing: not every brand-name drug has a generic yet. Some are still under patent, others are too complex to copy easily. That’s why you’ll find guides comparing brand-name drugs to their alternatives—like how Compazine stacks up against other anti-nausea meds, or how Careprost compares to Latisse for eyelash growth. These comparisons help you understand what you’re really paying for. Are you paying for reliability? For customer support? Or just for a name on the bottle?
And it’s not just about cost. Some people stick with brand-name drugs because they trust the manufacturer, or their doctor recommends it. Others switch to generics to save money—sometimes hundreds of dollars a month. The key is knowing that both options are safe. The FDA doesn’t let generics cut corners. They must match the brand in strength, dosage, and how fast they work in your body. If you’ve ever wondered why your prescription changed from Tylenol to acetaminophen, or from Nolvadex to tamoxifen, it’s not a mistake. It’s the system working as intended.
What you’ll find in the posts below are real comparisons, real stories, and real advice about navigating this system. Whether you’re managing chronic pain, treating a skin condition, or just trying to stretch your budget, you’ll see how brand-name drugs fit into the bigger picture of medication choices. No fluff. No marketing. Just clear, practical info to help you make smarter decisions about what’s in your medicine cabinet.

How to Use Patient Assistance Programs When No Generic Medication Exists
When no generic version of your medication exists, patient assistance programs can cover 100% of the cost. Learn how to apply, what documents you need, and how to overcome common barriers like accumulator programs and Medicare restrictions.
Why Generic Drugs Look Different from Brand-Name Medicines
Generic drugs look different from brand-name pills because of U.S. trademark laws - not because they're less effective. Learn why the color and shape change, how it affects safety, and what to do if you're confused by your new prescription.
Patient Trust: How to Build Confidence in Generic Medications
Generic medications are just as effective as brand-name drugs but cost up to 85% less. Learn why patients still distrust them-and how doctors, pharmacists, and the FDA are building real confidence in generics today.
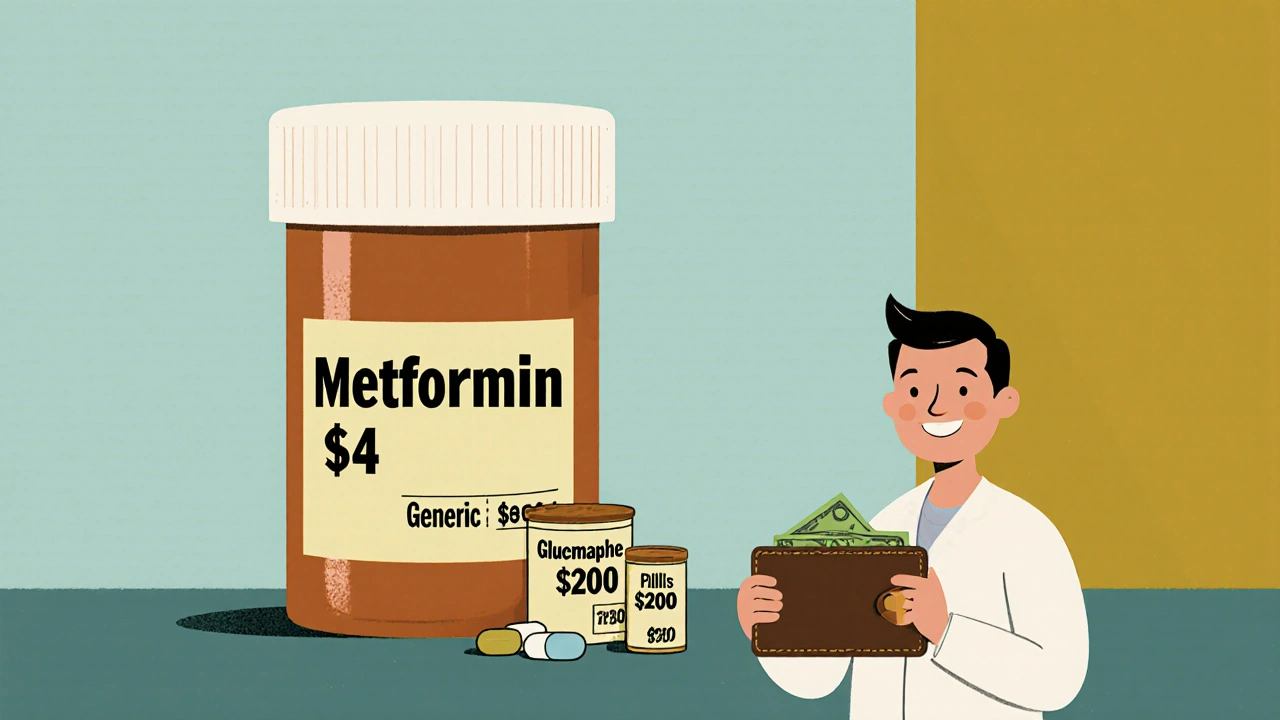
How Generics Control Healthcare Drug Spending: The Real Cost Savings
Generics make up 90% of U.S. prescriptions but only 12% of drug spending, saving $445 billion since 1984. Learn how they cut costs, why they’re safe, and what’s blocking even bigger savings.
